Monday Poster Session
Category: IBD
P2723 - A Diagnostic Dilemma: Abdominal Tuberculosis Mimicking Suspected Crohn’s Disease or Latent Tuberculosis Activated by Biologic Therapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anthony J. Papale, MD
North Shore University Hospital/Zucker School of Medicine at Hofstra University
Manhasset, NY
Presenting Author(s)
Award: Presidential Poster Award
Anthony J. Papale, MD1, Harrison Labban, MS2, Michael Delicce, MD3, Keith Sultan, MD, FACG4
1North Shore University Hospital/Zucker School of Medicine at Hofstra University, Manhasset, NY; 2Zucker School of Medicine Hofstra University, Manhasset, NY; 3Northwell Health, New Hyde Park, NY; 4Northwell Health, Manhasset, NY
Introduction: Abdominal tuberculosis (ATB) is a rare extrapulmonary manifestation of tuberculosis (TB) that represents approximately 1-3% of all cases. ATB presents with various signs and symptoms including abdominal pain, weight loss, fever, ascites, and bleeding, which often mimic conditions like inflammatory bowel disease (IBD) or malignancy. This mimicry poses a diagnostic challenge for clinicians and requires timely diagnosis and treatment, as the mortality rate for untreated disease is nearly 60%. We present a case of seronegative ATB that exemplifies this struggle and emphasizes the need for maintaining a broad differential when managing a patient with suspected IBD.
Case Description/Methods: A 51-year-old Asian male with Crohn’s Disease (CD) presented with 1 week of abdominal pain, fever, nausea, and non-bloody diarrhea. CD was diagnosed several months prior by colonoscopy showing predominant ileal involvement with biopsies demonstrating chronic focal active ileitis. After a negative QuantiFERON (QFN) assay, infliximab was started with minimal improvement of symptoms despite three months of therapy. On this hospitalization his exam was notable for diffuse abdominal tenderness and distension. Abdominal CT showed moderate ascites with nodularity along the omental fat. QFN was repeated and again negative. He underwent paracentesis which resulted in a negative acid-fast bacilli (AFB) smear but elevated adenosine deaminase. Omental nodule biopsy showed non-necrotizing granulomatous inflammation with negative AFB smear and eventually grew TB. He was deemed to have tuberculous peritonitis and initiated on a 9-month course of rifampin, INH, pyridoxine, and ethambutol. He had near full recovery after 6 months of treatment; repeat imaging and colonoscopy with biopsy were normal appearing with no evidence of CD or colitis, confirming TB as the etiology of disease.
Discussion: This case highlights the necessity to maintain a broad differential diagnosis and consider mimickers of IBD when establishing a diagnosis of Crohn’s Disease. Although the phenomenon of ATB imitating CD is well known, this presentation is particularly unique given the multiple negative QFN and AFB smears. Furthermore, non-necrotizing granulomas were observed on this patient’s biopsies rather than the caseating granulomas expected in TB. Due to the risk of false negative QFN testing, ATB should always be considered in patients presenting with symptoms suggestive of IBD, particularly in patients from endemic areas or high-risk populations.

Disclosures:
Anthony J. Papale, MD1, Harrison Labban, MS2, Michael Delicce, MD3, Keith Sultan, MD, FACG4. P2723 - A Diagnostic Dilemma: Abdominal Tuberculosis Mimicking Suspected Crohn’s Disease or Latent Tuberculosis Activated by Biologic Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Anthony J. Papale, MD1, Harrison Labban, MS2, Michael Delicce, MD3, Keith Sultan, MD, FACG4
1North Shore University Hospital/Zucker School of Medicine at Hofstra University, Manhasset, NY; 2Zucker School of Medicine Hofstra University, Manhasset, NY; 3Northwell Health, New Hyde Park, NY; 4Northwell Health, Manhasset, NY
Introduction: Abdominal tuberculosis (ATB) is a rare extrapulmonary manifestation of tuberculosis (TB) that represents approximately 1-3% of all cases. ATB presents with various signs and symptoms including abdominal pain, weight loss, fever, ascites, and bleeding, which often mimic conditions like inflammatory bowel disease (IBD) or malignancy. This mimicry poses a diagnostic challenge for clinicians and requires timely diagnosis and treatment, as the mortality rate for untreated disease is nearly 60%. We present a case of seronegative ATB that exemplifies this struggle and emphasizes the need for maintaining a broad differential when managing a patient with suspected IBD.
Case Description/Methods: A 51-year-old Asian male with Crohn’s Disease (CD) presented with 1 week of abdominal pain, fever, nausea, and non-bloody diarrhea. CD was diagnosed several months prior by colonoscopy showing predominant ileal involvement with biopsies demonstrating chronic focal active ileitis. After a negative QuantiFERON (QFN) assay, infliximab was started with minimal improvement of symptoms despite three months of therapy. On this hospitalization his exam was notable for diffuse abdominal tenderness and distension. Abdominal CT showed moderate ascites with nodularity along the omental fat. QFN was repeated and again negative. He underwent paracentesis which resulted in a negative acid-fast bacilli (AFB) smear but elevated adenosine deaminase. Omental nodule biopsy showed non-necrotizing granulomatous inflammation with negative AFB smear and eventually grew TB. He was deemed to have tuberculous peritonitis and initiated on a 9-month course of rifampin, INH, pyridoxine, and ethambutol. He had near full recovery after 6 months of treatment; repeat imaging and colonoscopy with biopsy were normal appearing with no evidence of CD or colitis, confirming TB as the etiology of disease.
Discussion: This case highlights the necessity to maintain a broad differential diagnosis and consider mimickers of IBD when establishing a diagnosis of Crohn’s Disease. Although the phenomenon of ATB imitating CD is well known, this presentation is particularly unique given the multiple negative QFN and AFB smears. Furthermore, non-necrotizing granulomas were observed on this patient’s biopsies rather than the caseating granulomas expected in TB. Due to the risk of false negative QFN testing, ATB should always be considered in patients presenting with symptoms suggestive of IBD, particularly in patients from endemic areas or high-risk populations.

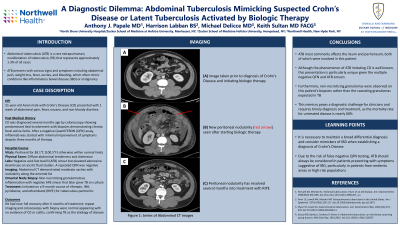
Figure: Figure 1: This series of axial images from abdominal CT demonstrates progression of the patient’s disease. The first (A) was taken prior to receiving a diagnosis of CD and initiating biologic therapy. Note how peritoneal nodularity (red arrows) can be appreciated on repeat imaging (B) from hospitalization but is resolved as seen on CT (C) performed several months into RIPE therapy.
Disclosures:
Anthony Papale indicated no relevant financial relationships.
Harrison Labban indicated no relevant financial relationships.
Michael Delicce indicated no relevant financial relationships.
Keith Sultan indicated no relevant financial relationships.
Anthony J. Papale, MD1, Harrison Labban, MS2, Michael Delicce, MD3, Keith Sultan, MD, FACG4. P2723 - A Diagnostic Dilemma: Abdominal Tuberculosis Mimicking Suspected Crohn’s Disease or Latent Tuberculosis Activated by Biologic Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

