Monday Poster Session
Category: IBD
P2729 - Extensive Venous Sinus Thrombosis After Oral Contraceptive Use in an Undiagnosed Ulcerative Colitis Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anudeeksha Satheeshkumar, MD
University of Texas Health Sciences Center
San Antonio, TX
Presenting Author(s)
Kyle Bandy, BA1, Anudeeksha Satheeshkumar, MD2, Sushreyta Rose, DO2, Christine Andre, MD2
1University of Texas Health Sciences Center, Long School of Medicine, San Antonio, TX; 2University of Texas Health Sciences Center, San Antonio, TX
Introduction: Hypercoagulability is an uncommon extraintestinal manifestation of inflammatory bowel disease (IBD); however, hypercoagulable events have been rarely reported as its initial presentation. Patients with active disease have been found to have an increased risk of thromboembolism, both venous and arterial. Here we present a unique case of initial presentation with extensive dural venous sinus thrombosis after the recent initiation of oral contraceptives (OCP) in a patient with undiagnosed IBD.
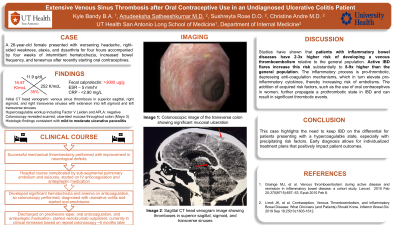
Case Description/Methods: A 26-year-old female presented with four hours of worsening headache, right-sided weakness, ataxia, and dysarthria, accompanied by four weeks of hematochezia, after recently starting OCPs. CT imaging revealed venous sinus thromboses in the superior sagittal, right and left sigmoid, and right and left transverse sinuses. Successful mechanical thrombectomy was performed with improvement in neurological deficits. The patient's hospital course was complicated by sub-segmental pulmonary embolism and seizures. She was started on anticoagulation with a heparin drip, however given ongoing hematochezia, GI was consulted and a colonoscopy was performed, which revealed scarred, ulcerated colonic mucosa. Histologic findings were consistent with mild to moderate ulcerative pancolitis. The patient was discharged on a steroid taper and initiated treatment with biologics outpatient with improvement in overall symptoms.
Discussion: Studies have shown that patients with IBD are at a 2-3x higher risk of developing venous thromboembolism relative to the general population, and active disease flares further increase this risk substantially to 8-9x1. The inflammatory process is pro-thrombotic, depressing natural anti-coagulation mechanisms and elevating pro-inflammatory cytokines, thus increasing the risk of embolisms. This, in addition to acquired risk factors such as oral contraceptive use, has been found to create a prothrombotic state in IBD2. This case highlights the need to keep IBD on the differential for patients presenting with a hypercoagulable state, especially when combined with precipitating risk factors.
1. Grainge MJ, et al. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010 Feb 20;375(9715):657-63. Epub 2010 Feb 8.
2. Limdi JK, et al. Contraception, Venous Thromboembolism, and Inflammatory Bowel Disease: What Clinicians (and Patients) Should Know. Inflamm Bowel Dis. 2019 Sep 18;25(10):1603-1612.

Disclosures:
Kyle Bandy, BA1, Anudeeksha Satheeshkumar, MD2, Sushreyta Rose, DO2, Christine Andre, MD2. P2729 - Extensive Venous Sinus Thrombosis After Oral Contraceptive Use in an Undiagnosed Ulcerative Colitis Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health Sciences Center, Long School of Medicine, San Antonio, TX; 2University of Texas Health Sciences Center, San Antonio, TX
Introduction: Hypercoagulability is an uncommon extraintestinal manifestation of inflammatory bowel disease (IBD); however, hypercoagulable events have been rarely reported as its initial presentation. Patients with active disease have been found to have an increased risk of thromboembolism, both venous and arterial. Here we present a unique case of initial presentation with extensive dural venous sinus thrombosis after the recent initiation of oral contraceptives (OCP) in a patient with undiagnosed IBD.
Case Description/Methods: A 26-year-old female presented with four hours of worsening headache, right-sided weakness, ataxia, and dysarthria, accompanied by four weeks of hematochezia, after recently starting OCPs. CT imaging revealed venous sinus thromboses in the superior sagittal, right and left sigmoid, and right and left transverse sinuses. Successful mechanical thrombectomy was performed with improvement in neurological deficits. The patient's hospital course was complicated by sub-segmental pulmonary embolism and seizures. She was started on anticoagulation with a heparin drip, however given ongoing hematochezia, GI was consulted and a colonoscopy was performed, which revealed scarred, ulcerated colonic mucosa. Histologic findings were consistent with mild to moderate ulcerative pancolitis. The patient was discharged on a steroid taper and initiated treatment with biologics outpatient with improvement in overall symptoms.
Discussion: Studies have shown that patients with IBD are at a 2-3x higher risk of developing venous thromboembolism relative to the general population, and active disease flares further increase this risk substantially to 8-9x1. The inflammatory process is pro-thrombotic, depressing natural anti-coagulation mechanisms and elevating pro-inflammatory cytokines, thus increasing the risk of embolisms. This, in addition to acquired risk factors such as oral contraceptive use, has been found to create a prothrombotic state in IBD2. This case highlights the need to keep IBD on the differential for patients presenting with a hypercoagulable state, especially when combined with precipitating risk factors.
1. Grainge MJ, et al. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010 Feb 20;375(9715):657-63. Epub 2010 Feb 8.
2. Limdi JK, et al. Contraception, Venous Thromboembolism, and Inflammatory Bowel Disease: What Clinicians (and Patients) Should Know. Inflamm Bowel Dis. 2019 Sep 18;25(10):1603-1612.

Figure: Image A. Colonoscopic image of the transverse colon showing significant mucosal ulceration
Image B. Colonoscopic image of the ascending colon showing mucosal ulceration
Image C. Another colonoscopic image of the ascending colon showing mucosal ulceration
Image D. Coronal CT image showing thromboses in super sagittal sinus and left transverse sinus
Image E. Sagittal CT venogram image showing thrombosis in superior sagittal sinus
Image F. Sagittal CT venogram image showing thromboses in superior sagittal, sigmoid, and transverse sinuses
Image B. Colonoscopic image of the ascending colon showing mucosal ulceration
Image C. Another colonoscopic image of the ascending colon showing mucosal ulceration
Image D. Coronal CT image showing thromboses in super sagittal sinus and left transverse sinus
Image E. Sagittal CT venogram image showing thrombosis in superior sagittal sinus
Image F. Sagittal CT venogram image showing thromboses in superior sagittal, sigmoid, and transverse sinuses
Disclosures:
Kyle Bandy indicated no relevant financial relationships.
Anudeeksha Satheeshkumar indicated no relevant financial relationships.
Sushreyta Rose indicated no relevant financial relationships.
Christine Andre indicated no relevant financial relationships.
Kyle Bandy, BA1, Anudeeksha Satheeshkumar, MD2, Sushreyta Rose, DO2, Christine Andre, MD2. P2729 - Extensive Venous Sinus Thrombosis After Oral Contraceptive Use in an Undiagnosed Ulcerative Colitis Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

