Monday Poster Session
Category: IBD
P2644 - Validation of Endoscopic Scoring System for Immune Checkpoint Inhibitor Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YW
Yinghong Wang, MD, PhD
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Yinghong Wang, MD, PhD1, Malek Satila, MD2, Carolina Colli Cruz, MD2, Krishnavathana Varatharajalu, MD3, Andres Rivera, MD4, Kian Abdul-Baki, DO5, Kei Takigawa, MD4, Tanvi Gupta, MD6, Elliot Axel. Baerman, MD4, Linfeng Lu, MD4, Irene J. Lee, MD4, Hamza Salim, MD5, Raakhi Menon, DO5, Andrew Sullivan, MD7, Varun Vemulapalli, MD6, Cristina M. Natha, MD6, Ayesha Khan, DO5
1University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3The University of Texas MD Anderson Cancer Center, Houston, TX; 4Baylor College of Medicine, Houston, TX; 5University of Texas Medical Branch, Galveston, TX; 6University of Texas Health, McGovern Medical School, Houston, TX; 7University of Texas Health Science Center, Houston, TX
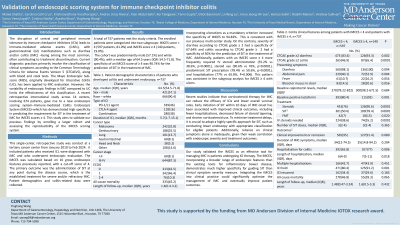
Introduction: Immune-mediated colitis (IMC) is a dreaded toxicity of immune-checkpoint inhibition (ICI) that often leads to treatment discontinuation. The endoscopic scoring systems used for this disease are adapted from inflammatory bowel disease practice but fail to capture the full spectrum of disease. The IMC endoscopic score (IMCES) was proposed as a new scoring system to help guide treatment. This study aims to validate the IMCES and explore its association with other IMC outcomes.
Methods: This was a single-center, retrospective study including all patients who received ICI and were diagnosed with IMC, who also underwent endoscopic evaluation. The IMCES was calculated based on 10 gross endoscopic features reported in the previous study, and the same score cut-off of 4 was used. We collected patient demographic information as well as colitis clinical and endoscopic data.
Results: 709 patients met the study criteria, 610 with an IMCES score less than 4 (86.0%), and 99 (14.0%) with a score ≥ 4. Patients were predominantly white (90.6%) and male (57.0%), with a median age of 64 (IQR: 54-72). IMCES scores of 4 and above were found to have a specificity of 90% for future SIT use, which increased to 95.5% after including ulcers as a mandatory score criterion. This is compared to clinical symptoms of diarrhea grade 2 and above, which had a specificity of 28.1% and colitis, which had a specificity of 63.0%. These patients had a more severe presentation of IMC with a higher rate of grade 2 and above diarrhea (93.8% of those with IMCES ≥ 4 vs. 84.6% of those with IMCES < 4; p=0.01) and colitis (62.4% vs. 48.4%; p=0.01), more frequent abdominal pain (54.4% vs. 38.2%; p=0.002), and positive stool biomarkers (93.3% vs. 79.2% for fecal lactoferrin, median of 582 vs. 124 for calprotectin; p< 0.05 for both). Patients with an IMCES ≥4 more frequently required steroid (90.9% vs 76.7%, P=0.001), and hospitalization (82.8% vs 66%, P=0.001) as well. Adding ulcers as a mandatory criterion for scores ≥ 4 led to more prominent differences in the above parameters.
Discussion: This study provided was a follow-up to our previously proposed endoscopic scoring system offering a validation of the IMCES. We confirmed that while clinical symptoms had a low specificity for future SIT use, an IMCES cut-off of 4 and above has a high specificity for SIT use (90%) and was associated with a worse disease course, supporting the value of endoscopic evaluation for IMC.
Disclosures:
Yinghong Wang, MD, PhD1, Malek Satila, MD2, Carolina Colli Cruz, MD2, Krishnavathana Varatharajalu, MD3, Andres Rivera, MD4, Kian Abdul-Baki, DO5, Kei Takigawa, MD4, Tanvi Gupta, MD6, Elliot Axel. Baerman, MD4, Linfeng Lu, MD4, Irene J. Lee, MD4, Hamza Salim, MD5, Raakhi Menon, DO5, Andrew Sullivan, MD7, Varun Vemulapalli, MD6, Cristina M. Natha, MD6, Ayesha Khan, DO5. P2644 - Validation of Endoscopic Scoring System for Immune Checkpoint Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3The University of Texas MD Anderson Cancer Center, Houston, TX; 4Baylor College of Medicine, Houston, TX; 5University of Texas Medical Branch, Galveston, TX; 6University of Texas Health, McGovern Medical School, Houston, TX; 7University of Texas Health Science Center, Houston, TX
Introduction: Immune-mediated colitis (IMC) is a dreaded toxicity of immune-checkpoint inhibition (ICI) that often leads to treatment discontinuation. The endoscopic scoring systems used for this disease are adapted from inflammatory bowel disease practice but fail to capture the full spectrum of disease. The IMC endoscopic score (IMCES) was proposed as a new scoring system to help guide treatment. This study aims to validate the IMCES and explore its association with other IMC outcomes.
Methods: This was a single-center, retrospective study including all patients who received ICI and were diagnosed with IMC, who also underwent endoscopic evaluation. The IMCES was calculated based on 10 gross endoscopic features reported in the previous study, and the same score cut-off of 4 was used. We collected patient demographic information as well as colitis clinical and endoscopic data.
Results: 709 patients met the study criteria, 610 with an IMCES score less than 4 (86.0%), and 99 (14.0%) with a score ≥ 4. Patients were predominantly white (90.6%) and male (57.0%), with a median age of 64 (IQR: 54-72). IMCES scores of 4 and above were found to have a specificity of 90% for future SIT use, which increased to 95.5% after including ulcers as a mandatory score criterion. This is compared to clinical symptoms of diarrhea grade 2 and above, which had a specificity of 28.1% and colitis, which had a specificity of 63.0%. These patients had a more severe presentation of IMC with a higher rate of grade 2 and above diarrhea (93.8% of those with IMCES ≥ 4 vs. 84.6% of those with IMCES < 4; p=0.01) and colitis (62.4% vs. 48.4%; p=0.01), more frequent abdominal pain (54.4% vs. 38.2%; p=0.002), and positive stool biomarkers (93.3% vs. 79.2% for fecal lactoferrin, median of 582 vs. 124 for calprotectin; p< 0.05 for both). Patients with an IMCES ≥4 more frequently required steroid (90.9% vs 76.7%, P=0.001), and hospitalization (82.8% vs 66%, P=0.001) as well. Adding ulcers as a mandatory criterion for scores ≥ 4 led to more prominent differences in the above parameters.
Discussion: This study provided was a follow-up to our previously proposed endoscopic scoring system offering a validation of the IMCES. We confirmed that while clinical symptoms had a low specificity for future SIT use, an IMCES cut-off of 4 and above has a high specificity for SIT use (90%) and was associated with a worse disease course, supporting the value of endoscopic evaluation for IMC.
Disclosures:
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Malek Satila indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Andres Rivera indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Kei Takigawa indicated no relevant financial relationships.
Tanvi Gupta indicated no relevant financial relationships.
Elliot Baerman indicated no relevant financial relationships.
Linfeng Lu indicated no relevant financial relationships.
Irene Lee indicated no relevant financial relationships.
Hamza Salim indicated no relevant financial relationships.
Raakhi Menon indicated no relevant financial relationships.
Andrew Sullivan indicated no relevant financial relationships.
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Yinghong Wang, MD, PhD1, Malek Satila, MD2, Carolina Colli Cruz, MD2, Krishnavathana Varatharajalu, MD3, Andres Rivera, MD4, Kian Abdul-Baki, DO5, Kei Takigawa, MD4, Tanvi Gupta, MD6, Elliot Axel. Baerman, MD4, Linfeng Lu, MD4, Irene J. Lee, MD4, Hamza Salim, MD5, Raakhi Menon, DO5, Andrew Sullivan, MD7, Varun Vemulapalli, MD6, Cristina M. Natha, MD6, Ayesha Khan, DO5. P2644 - Validation of Endoscopic Scoring System for Immune Checkpoint Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
