Monday Poster Session
Category: IBD
P2648 - Treatment Outcomes of Prolonged Induction or Re-Escalation Dosing of Upadacitinib in Patients With Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Ellen Axenfeld, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Ellen Axenfeld, MD1, Vasantham Annadurai, MD1, Joseph Clinton, MD2, Michael Frohlinger, MD2, Lauren George, MD3, Adam S.. Faye, MD4, Raymond K. Cross, MD, MS, FACG5, Jordan Axelrad, MD, MPH4
1NYU Langone Health, New York, NY; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD; 4NYU Grossman School of Medicine, New York, NY; 5Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD
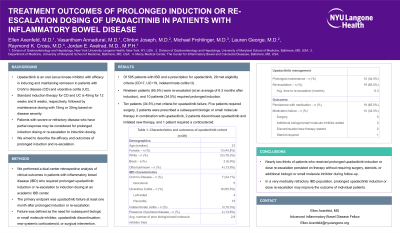
Introduction: Upadacitinib is an oral Janus kinase (JAK) inhibitor with efficacy in inducing and maintaining remission in patients with Crohn’s disease (CD) and ulcerative colitis (UC). Standard upadacitinib induction therapy for CD and UC is 45mg for 12 weeks and 8 weeks, respectively, followed by maintenance dosing with 15mg or 30mg based on disease severity. Patients with severe or refractory disease who have partial response may be considered for prolonged induction and/or re-escalation.
Methods: We performed a dual-center retrospective analysis of clinical outcomes in patients with inflammatory bowel disease (IBD) who required prolonged upadacitinib induction or re-escalation to induction dosing. The primary endpoint was upadacitinib failure at least one month after prolonged induction or re-escalation. Failure was defined as the need for subsequent biologic or small molecule inhibitor, upadacitinib discontinuation, new systemic corticosteroid, or surgical intervention.
Results: Of 595 patients with IBD and a prescription for upadacitinib, 29 met eligibility criteria (CD=7, UC=19, indeterminate colitis=3, Table) with adequate follow-up data. The majority were white (n=23, 79.3%) and male (n=16, 55.2%). At upadacitinib initiation, the median age was 31 years (IQR=15 years) and patients had a median IBD duration of 7.9 years (IQR=10 years) with prior exposure to 3 advanced therapies, on average. Of the 29 patients, 19 patients (65.5%) were re-escalated (at an average of 8.4 months after induction), and 10 patients (34.5%) required prolonged induction. Ten patients (34.5%) met criteria for upadacitinib failure. Five patients required surgery, two patients were prescribed a subsequent biologic or small molecule therapy in combination with upadacitinib, two patients discontinued upadacitinib and initiated new therapy, and one required a corticosteroid. The only adverse medication effect was acne in one patient.
Discussion: Over two-thirds of patients who received prolonged upadacitinib induction or dose re-escalation persisted on therapy after at least one month without requiring surgery, steroids, or additional biologic or small molecule inhibitor. In a very medically refractory IBD population, prolonged upadacitinib induction or dose re-escalation may improve the outcome of individual patients. Additional and prospective long-term data is required to confirm our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ellen Axenfeld, MD1, Vasantham Annadurai, MD1, Joseph Clinton, MD2, Michael Frohlinger, MD2, Lauren George, MD3, Adam S.. Faye, MD4, Raymond K. Cross, MD, MS, FACG5, Jordan Axelrad, MD, MPH4. P2648 - Treatment Outcomes of Prolonged Induction or Re-Escalation Dosing of Upadacitinib in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland School of Medicine, Baltimore, MD; 4NYU Grossman School of Medicine, New York, NY; 5Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD
Introduction: Upadacitinib is an oral Janus kinase (JAK) inhibitor with efficacy in inducing and maintaining remission in patients with Crohn’s disease (CD) and ulcerative colitis (UC). Standard upadacitinib induction therapy for CD and UC is 45mg for 12 weeks and 8 weeks, respectively, followed by maintenance dosing with 15mg or 30mg based on disease severity. Patients with severe or refractory disease who have partial response may be considered for prolonged induction and/or re-escalation.
Methods: We performed a dual-center retrospective analysis of clinical outcomes in patients with inflammatory bowel disease (IBD) who required prolonged upadacitinib induction or re-escalation to induction dosing. The primary endpoint was upadacitinib failure at least one month after prolonged induction or re-escalation. Failure was defined as the need for subsequent biologic or small molecule inhibitor, upadacitinib discontinuation, new systemic corticosteroid, or surgical intervention.
Results: Of 595 patients with IBD and a prescription for upadacitinib, 29 met eligibility criteria (CD=7, UC=19, indeterminate colitis=3, Table) with adequate follow-up data. The majority were white (n=23, 79.3%) and male (n=16, 55.2%). At upadacitinib initiation, the median age was 31 years (IQR=15 years) and patients had a median IBD duration of 7.9 years (IQR=10 years) with prior exposure to 3 advanced therapies, on average. Of the 29 patients, 19 patients (65.5%) were re-escalated (at an average of 8.4 months after induction), and 10 patients (34.5%) required prolonged induction. Ten patients (34.5%) met criteria for upadacitinib failure. Five patients required surgery, two patients were prescribed a subsequent biologic or small molecule therapy in combination with upadacitinib, two patients discontinued upadacitinib and initiated new therapy, and one required a corticosteroid. The only adverse medication effect was acne in one patient.
Discussion: Over two-thirds of patients who received prolonged upadacitinib induction or dose re-escalation persisted on therapy after at least one month without requiring surgery, steroids, or additional biologic or small molecule inhibitor. In a very medically refractory IBD population, prolonged upadacitinib induction or dose re-escalation may improve the outcome of individual patients. Additional and prospective long-term data is required to confirm our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ellen Axenfeld indicated no relevant financial relationships.
Vasantham Annadurai indicated no relevant financial relationships.
Joseph Clinton indicated no relevant financial relationships.
Michael Frohlinger indicated no relevant financial relationships.
Lauren George: Janssen – Advisory Committee/Board Member.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Raymond Cross: AbbVie – Consultant. Adiso – Consultant. Bristol Myers Squibb – Consultant. CorEvitas Registry – Scientific co-director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – Executive committee member. Janssen – Consultant, Grant/Research Support. Magellan Health – Consultant. Option Care Health – Consultant. Pfizer – Consultant. Pharmacosmos – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant. Sebela – Consultant. Takeda – Consultant.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Ellen Axenfeld, MD1, Vasantham Annadurai, MD1, Joseph Clinton, MD2, Michael Frohlinger, MD2, Lauren George, MD3, Adam S.. Faye, MD4, Raymond K. Cross, MD, MS, FACG5, Jordan Axelrad, MD, MPH4. P2648 - Treatment Outcomes of Prolonged Induction or Re-Escalation Dosing of Upadacitinib in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
