Monday Poster Session
Category: IBD
P2650 - Prevalence of Persistent Gastrointestinal Symptoms in IBD Patients with Endoscopically Quiescent Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carl Samaha, MD
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Carl Samaha, MD, Jeffrey Dueker, MD, MPH, Elyse Johnston, MD, Marc Schwartz, MD, David Binion, MD, Richard Duerr, MD, Amir Ghaffari, MD, PhD
University of Pittsburgh Medical Center, Pittsburgh, PA
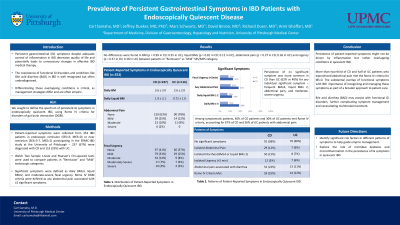
Introduction: Persistent gastrointestinal (GI) symptoms despite adequate control of inflammation in IBD poses a challenge for clinical management. Ameliorating persistent GI symptoms no longer related to active inflammation can improve quality of life and potentially avoid unnecessary changes in effective IBD medical therapy. We sought to define the spectrum of persistent GI symptoms, including loose stools, abdominal pain and fecal urgency despite achieving endoscopic remission in a prospective cohort of IBD patients.
Methods: Data from 353 University of Pittsburgh SPARC-IBD participants in endoscopic remission (Simple endoscopic score (SES)< 3, Mayo Endoscopic Score (MES)=0) or near remission (SES=3-7, MES=1) – 237 (67%) were diagnosed with CD and 116 (33%) with UC. Patient-reported symptoms at colonoscopy were extracted. Welch Two Sample t-tests and Pearson's Chi-squared tests were used to compare patients in "Remission" and "Mild" endoscopic categories. Significant symptoms were defined as daily BM≥4, liquid BM≥2, and moderate-severe fecal urgency. Rome IV DGBI criteria included any abdominal pain associated with ≥2 significant symptoms. Descriptive statistics were calculated and presented as means (± STD) or frequencies.
Results: No differences were found in BM (p = 0.99 in CD; 0.35 in UC), liquid BMs (p = 0.81 in CD; 0.12 in UC), abdominal pain (p = 0.37 in CD; 0.36 in UC) and urgency (p = 0.37 in CD; 0.18 in UC) between patients in "Remission" vs "Mild" SES/MES category. Persistence of ≥1 significant symptom was more common in CD than UC (62% vs 40%) for any individual symptoms – frequent BM≥4 (38% vs 16%), liquid BM≥ 2 (24% vs 15%), abdominal pain (37% vs 21%), and moderate-severe urgency (26% vs 17%). Among symptomatic patients, 40% of CD and 30% of UC patients met Rome IV criteria, or 67% of CD and 56% of UC patients with abdominal pain. Isolated pain was seen in 12% of CD and 6% of UC patients. Isolated diarrhea (BM≥4 or liquid BM≥2) was prevalent in 21% of CD and 7% of UC patients. Isolated urgency rates were similar in both CD and UC (5% vs 6%).
Discussion: A subgroup of IBD patients in endoscopic remission suffer from IBS-like symptoms, particularly in CD, independent of inflammation. Further work characterizing risk factors for persistent GI symptoms and palliative approaches despite control of IBD mucosal inflammation is needed to improve patients quality of life.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carl Samaha, MD, Jeffrey Dueker, MD, MPH, Elyse Johnston, MD, Marc Schwartz, MD, David Binion, MD, Richard Duerr, MD, Amir Ghaffari, MD, PhD. P2650 - Prevalence of Persistent Gastrointestinal Symptoms in IBD Patients with Endoscopically Quiescent Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Persistent gastrointestinal (GI) symptoms despite adequate control of inflammation in IBD poses a challenge for clinical management. Ameliorating persistent GI symptoms no longer related to active inflammation can improve quality of life and potentially avoid unnecessary changes in effective IBD medical therapy. We sought to define the spectrum of persistent GI symptoms, including loose stools, abdominal pain and fecal urgency despite achieving endoscopic remission in a prospective cohort of IBD patients.
Methods: Data from 353 University of Pittsburgh SPARC-IBD participants in endoscopic remission (Simple endoscopic score (SES)< 3, Mayo Endoscopic Score (MES)=0) or near remission (SES=3-7, MES=1) – 237 (67%) were diagnosed with CD and 116 (33%) with UC. Patient-reported symptoms at colonoscopy were extracted. Welch Two Sample t-tests and Pearson's Chi-squared tests were used to compare patients in "Remission" and "Mild" endoscopic categories. Significant symptoms were defined as daily BM≥4, liquid BM≥2, and moderate-severe fecal urgency. Rome IV DGBI criteria included any abdominal pain associated with ≥2 significant symptoms. Descriptive statistics were calculated and presented as means (± STD) or frequencies.
Results: No differences were found in BM (p = 0.99 in CD; 0.35 in UC), liquid BMs (p = 0.81 in CD; 0.12 in UC), abdominal pain (p = 0.37 in CD; 0.36 in UC) and urgency (p = 0.37 in CD; 0.18 in UC) between patients in "Remission" vs "Mild" SES/MES category. Persistence of ≥1 significant symptom was more common in CD than UC (62% vs 40%) for any individual symptoms – frequent BM≥4 (38% vs 16%), liquid BM≥ 2 (24% vs 15%), abdominal pain (37% vs 21%), and moderate-severe urgency (26% vs 17%). Among symptomatic patients, 40% of CD and 30% of UC patients met Rome IV criteria, or 67% of CD and 56% of UC patients with abdominal pain. Isolated pain was seen in 12% of CD and 6% of UC patients. Isolated diarrhea (BM≥4 or liquid BM≥2) was prevalent in 21% of CD and 7% of UC patients. Isolated urgency rates were similar in both CD and UC (5% vs 6%).
Discussion: A subgroup of IBD patients in endoscopic remission suffer from IBS-like symptoms, particularly in CD, independent of inflammation. Further work characterizing risk factors for persistent GI symptoms and palliative approaches despite control of IBD mucosal inflammation is needed to improve patients quality of life.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carl Samaha indicated no relevant financial relationships.
Jeffrey Dueker indicated no relevant financial relationships.
Elyse Johnston indicated no relevant financial relationships.
Marc Schwartz indicated no relevant financial relationships.
David Binion: Abbvie – Grant/Research Support. Merck – Grant/Research Support. Takeda – Grant/Research Support.
Richard Duerr indicated no relevant financial relationships.
Amir Ghaffari indicated no relevant financial relationships.
Carl Samaha, MD, Jeffrey Dueker, MD, MPH, Elyse Johnston, MD, Marc Schwartz, MD, David Binion, MD, Richard Duerr, MD, Amir Ghaffari, MD, PhD. P2650 - Prevalence of Persistent Gastrointestinal Symptoms in IBD Patients with Endoscopically Quiescent Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
