Monday Poster Session
Category: IBD
P2653 - Recapturing Response and Remission With Short-Term Upadacitinib Dose Escalation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Meghana Golla, MD
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Meghana Golla, MD1, Sara N. Horst, MD2, Audrey Bennett, MD1, Patrick Nichols, PharmD2, Cameron Fawcett, 2, Elizabeth A. Scoville, MD, MSCI1, Baldeep Pabla, MD, MSCI2, Robin Dalal, MD1, Dawn Beaulieu, MD2, David Schwartz, MD3
1Vanderbilt University Medical Center, Nashville, TN; 2Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 3VUMC, Nashville, TN
Introduction: Upadacitinib is a selective oral JAK inhibitor approved for the induction and maintenance of moderate to severe ulcerative colitis (UC) and Crohn’s disease (CD). Upadacitinib is initiated at an induction dose of 45 mg daily with maintenance doses of 30 mg or 15 mg daily. This study aimed to evaluate a temporary increase of upadacitinib to 45 mg daily for patients who lost response to lower maintenance dosing.
Methods: This was a retrospective study from a single tertiary care inflammatory bowel disease (IBD) center with clinical data and outcomes collected through chart review. Patients were included if: 1) they received induction dose of upadacitinib 45 mg daily for at least 1 month, 2) decreased to a maintenance dose of 30 or 15 mg, and 3) required dose escalation back to 45 mg daily because of increased symptoms, abnormal inflammatory markers, or endoscopic assessment. Statistical analysis was done using Wilcoxon signed-rank testing.
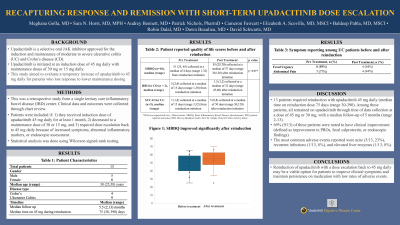
Results: 13 patients required reinduction with upadacitinib 45 mg daily (median time on reinduction dose 75 days (range 30-390). 61% were female, 69% had UC, 31% had CD, and median age was 38 years (range 25-58). Among these patients, all remained on upadacitinib through time of data collection at a dose of 45 mg or 30 mg, with a median follow-up of 5 months (range 2-13). Table 1 details patient reported outcomes (PROs). 69% (9/13) of these patients were noted to have clinical improvement (defined as improvement in PROs, fecal calprotectin, or endoscopic findings). For patients with UC, 8/9 (89%) reported fecal urgency and 7/9 (77%) reported abdominal pain prior to reinduction. After reinduction, 4/9 (44%) reported fecal urgency and 4/9 (44%) reported abdominal pain. The most common adverse events reported were acne (3/13, 23%), recurrent infections (1/13, 8%), and elevated liver enzymes (1/13, 8%).
Discussion: Reinduction of upadacitinib with a dose escalation back to 45 mg daily may be a viable option for patients to improve clinical symptoms and maintain persistence on medication with low rates of adverse events.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Meghana Golla, MD1, Sara N. Horst, MD2, Audrey Bennett, MD1, Patrick Nichols, PharmD2, Cameron Fawcett, 2, Elizabeth A. Scoville, MD, MSCI1, Baldeep Pabla, MD, MSCI2, Robin Dalal, MD1, Dawn Beaulieu, MD2, David Schwartz, MD3. P2653 - Recapturing Response and Remission With Short-Term Upadacitinib Dose Escalation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Vanderbilt University Medical Center, Nashville, TN; 2Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 3VUMC, Nashville, TN
Introduction: Upadacitinib is a selective oral JAK inhibitor approved for the induction and maintenance of moderate to severe ulcerative colitis (UC) and Crohn’s disease (CD). Upadacitinib is initiated at an induction dose of 45 mg daily with maintenance doses of 30 mg or 15 mg daily. This study aimed to evaluate a temporary increase of upadacitinib to 45 mg daily for patients who lost response to lower maintenance dosing.
Methods: This was a retrospective study from a single tertiary care inflammatory bowel disease (IBD) center with clinical data and outcomes collected through chart review. Patients were included if: 1) they received induction dose of upadacitinib 45 mg daily for at least 1 month, 2) decreased to a maintenance dose of 30 or 15 mg, and 3) required dose escalation back to 45 mg daily because of increased symptoms, abnormal inflammatory markers, or endoscopic assessment. Statistical analysis was done using Wilcoxon signed-rank testing.
Results: 13 patients required reinduction with upadacitinib 45 mg daily (median time on reinduction dose 75 days (range 30-390). 61% were female, 69% had UC, 31% had CD, and median age was 38 years (range 25-58). Among these patients, all remained on upadacitinib through time of data collection at a dose of 45 mg or 30 mg, with a median follow-up of 5 months (range 2-13). Table 1 details patient reported outcomes (PROs). 69% (9/13) of these patients were noted to have clinical improvement (defined as improvement in PROs, fecal calprotectin, or endoscopic findings). For patients with UC, 8/9 (89%) reported fecal urgency and 7/9 (77%) reported abdominal pain prior to reinduction. After reinduction, 4/9 (44%) reported fecal urgency and 4/9 (44%) reported abdominal pain. The most common adverse events reported were acne (3/13, 23%), recurrent infections (1/13, 8%), and elevated liver enzymes (1/13, 8%).
Discussion: Reinduction of upadacitinib with a dose escalation back to 45 mg daily may be a viable option for patients to improve clinical symptoms and maintain persistence on medication with low rates of adverse events.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Meghana Golla: .
Sara Horst: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Takeda – Consultant.
Audrey Bennett: Celltrion – Consultant.
Patrick Nichols: AbbVie – Advisory Committee/Board Member.
Cameron Fawcett indicated no relevant financial relationships.
Elizabeth Scoville indicated no relevant financial relationships.
Baldeep Pabla: Bristol Myers Squibb – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Ossium Health – Consultant. Pfzier – Advisory Committee/Board Member.
Robin Dalal: Abbvie – Consultant.
Dawn Beaulieu: Abbvie – Consultant. Bristol Myers Squibb – Consultant. Institute of functional medicine – Consultant. Takeda – Consultant.
David Schwartz: abbvie – Consultant. avbios – Advisory Committee/Board Member, Consultant. BMS – Consultant. janssen – Consultant. takeda – Consultant.
Meghana Golla, MD1, Sara N. Horst, MD2, Audrey Bennett, MD1, Patrick Nichols, PharmD2, Cameron Fawcett, 2, Elizabeth A. Scoville, MD, MSCI1, Baldeep Pabla, MD, MSCI2, Robin Dalal, MD1, Dawn Beaulieu, MD2, David Schwartz, MD3. P2653 - Recapturing Response and Remission With Short-Term Upadacitinib Dose Escalation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
