Monday Poster Session
Category: IBD
P2589 - Quality Improvement: VTE Prophylaxis for Inflammatory Bowel Disease Admissions - Room for Improvement
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kyle K. Meissner, MD, MBA
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Kyle Meissner, MD, MBA1, Lindsey Shipley, MD1, Dalton A.. Norwood, MD2, Mary Grace Cox, MPH1, Sebastian Pasara, MPH3, Kirk B.. Russ, MD1
1University of Alabama at Birmingham, Birmingham, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Patients with inflammatory bowel disease (IBD) are at an elevated risk for both venous and arterial thrombosis. This is increased with active disease, hospital admission and acute illness. We sought to evaluate the use of venous thromboembolism (VTE) prophylaxis in patients with IBD at our tertiary medical center.
Methods: This retrospective study analyzed admissions from 1/1/2020 to 12/31/2022 of adult patients with a diagnosis of IBD. Patients were excluded if they were on chronic anticoagulation, had length of stay less < 24 hours, and/or were admitted to an ambulatory or palliative care unit. Patients were divided into two subgroups, IBD flare and IBD admitted for other reasons. An IBD flare was defined as active disease as evidenced by elevated inflammatory markers (ESR, CRP), colonoscopy and/or cross-sectional imaging. We compared these two subgroups and analyzed VTE risk assessment, VTE prophylaxis administration, missed doses and reasons why, GI consultation (yes or no), and GI recommendations for VTE prophylaxis.
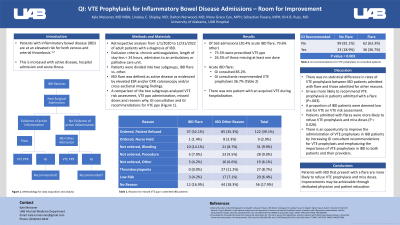
Results: Of 563 admissions, 75.5% were prescribed VTE prophylaxis with 26.5% of those missing at least one dose. The most common reason for missed doses is displayed in Table 1. 20.4% (N = 115) of the admissions reviewed were admitted with acute IBD flare and 79.6% (N = 448) were admitted for other reasons. In patients admitted with acute IBD flare, GI was consulted 85.2% versus 26.1% in IBD patients admitted for other reasons. GI consultants recommended VTE prophylaxis 36.7% of the time in acute IBD flares versus 18.9% in IBD patients admitted for other reasons. There was one patient with an acquired VTE during hospitalization.
Discussion: There was no statistical difference in rates of VTE prophylaxis between IBD patients admitted with flare and those admitted for other reasons. GI was more likely to recommend DVT prophylaxis in patients admitted with a flare (P=.003). A proportion of IBD patients were deemed low risk for VTE on VTE risk assessment, highlighting a lack of awareness amongst providers of the baseline elevated risk of VTE in IBD. Patients admitted with flares were more likely to refuse VTE prophylaxis and miss doses (P = 0.026). There is an opportunity to improve the administration of VTE prophylaxis in IBD patients by increasing GI consultant recommendations for VTE prophylaxis and emphasizing the importance of VTE prophylaxis in IBD to both patients and their providers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyle Meissner, MD, MBA1, Lindsey Shipley, MD1, Dalton A.. Norwood, MD2, Mary Grace Cox, MPH1, Sebastian Pasara, MPH3, Kirk B.. Russ, MD1. P2589 - Quality Improvement: VTE Prophylaxis for Inflammatory Bowel Disease Admissions - Room for Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Patients with inflammatory bowel disease (IBD) are at an elevated risk for both venous and arterial thrombosis. This is increased with active disease, hospital admission and acute illness. We sought to evaluate the use of venous thromboembolism (VTE) prophylaxis in patients with IBD at our tertiary medical center.
Methods: This retrospective study analyzed admissions from 1/1/2020 to 12/31/2022 of adult patients with a diagnosis of IBD. Patients were excluded if they were on chronic anticoagulation, had length of stay less < 24 hours, and/or were admitted to an ambulatory or palliative care unit. Patients were divided into two subgroups, IBD flare and IBD admitted for other reasons. An IBD flare was defined as active disease as evidenced by elevated inflammatory markers (ESR, CRP), colonoscopy and/or cross-sectional imaging. We compared these two subgroups and analyzed VTE risk assessment, VTE prophylaxis administration, missed doses and reasons why, GI consultation (yes or no), and GI recommendations for VTE prophylaxis.
Results: Of 563 admissions, 75.5% were prescribed VTE prophylaxis with 26.5% of those missing at least one dose. The most common reason for missed doses is displayed in Table 1. 20.4% (N = 115) of the admissions reviewed were admitted with acute IBD flare and 79.6% (N = 448) were admitted for other reasons. In patients admitted with acute IBD flare, GI was consulted 85.2% versus 26.1% in IBD patients admitted for other reasons. GI consultants recommended VTE prophylaxis 36.7% of the time in acute IBD flares versus 18.9% in IBD patients admitted for other reasons. There was one patient with an acquired VTE during hospitalization.
Discussion: There was no statistical difference in rates of VTE prophylaxis between IBD patients admitted with flare and those admitted for other reasons. GI was more likely to recommend DVT prophylaxis in patients admitted with a flare (P=.003). A proportion of IBD patients were deemed low risk for VTE on VTE risk assessment, highlighting a lack of awareness amongst providers of the baseline elevated risk of VTE in IBD. Patients admitted with flares were more likely to refuse VTE prophylaxis and miss doses (P = 0.026). There is an opportunity to improve the administration of VTE prophylaxis in IBD patients by increasing GI consultant recommendations for VTE prophylaxis and emphasizing the importance of VTE prophylaxis in IBD to both patients and their providers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyle Meissner indicated no relevant financial relationships.
Lindsey Shipley indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Mary Grace Cox indicated no relevant financial relationships.
Sebastian Pasara indicated no relevant financial relationships.
Kirk Russ indicated no relevant financial relationships.
Kyle Meissner, MD, MBA1, Lindsey Shipley, MD1, Dalton A.. Norwood, MD2, Mary Grace Cox, MPH1, Sebastian Pasara, MPH3, Kirk B.. Russ, MD1. P2589 - Quality Improvement: VTE Prophylaxis for Inflammatory Bowel Disease Admissions - Room for Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

