Monday Poster Session
Category: IBD
P2590 - Negative Illness Perceptions are Associated With Clinical Disease Activity in Adult Patients With Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Emily Sheng, BA
Hospital of the University of Pennsylvania
Philadelphia, PA
Presenting Author(s)
David Bickford, MD1, Emily Sheng, BA1, Melissa G. Hunt, PhD2, Sara N. Horst, MD3, Samir A. Shah, MD4, Sumona Saha, MD, MS5, Sasha Taleban, MD6, Lily Brown, PhD1, Kanika Malani, BS7, Megan Lutz, MD8, Hannah Fiske, MD9, Robert Kuehnel, PhD1, Brittaney Bonhomme, BA1, Alandra Weaver, MPH10, Millie D. Long, MD, MPH11, Raymond Cross, MD12, James Lewis, MD, MSCE13, Chung Sang Tse, MD2
1Hospital of the University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI; 5University of Wisconsin Hospitals and Clinics, Madison, WI; 6University of Arizona, Tucson, AZ; 7The Warren Alpert Medical School of Brown University, Providence, RI; 8University of Wisconsin-Madison, Madison, WI; 9Brown University / Rhode Island Hospital, Providence, RI; 10Crohn's and Colitis Foundation, New York, NY; 11Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 12University of Maryland School of Medicine, Baltimore, MD; 13Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA
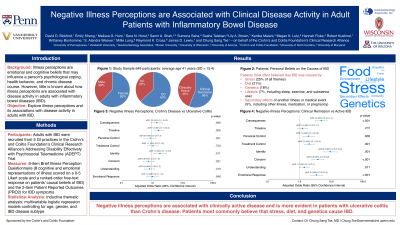
Introduction: Illness perceptions are emotional and cognitive beliefs that may influence a person’s psychological coping, health behavior, and chronic disease course. However, there is a knowledge gap for how illness perceptions are associated with disease activity in adults with inflammatory bowel diseases (IBD).
Methods: We conducted a mixed-methods survey study on adults with IBD from five geographically diverse gastroenterology practices participating in the Crohn’s and Colitis Foundation’s Clinical Research Alliance’s ADEPT Trial (NCT05635292). We used multivariable logistic regression models to assess for associations between negative illness perceptions and clinical disease activity (2-item patient-reported outcome, PRO-2), adjusted for age, gender, and IBD subtype. The Brief Illness Perception Questionnaire (BIPQ) assesses eight cognitive and emotional representations of IBD (0-5 Likert scale, cut points at >75th interquartile for negative illness perceptions, with reversed coding for positively worded items) and an open-ended question on patients’ personal beliefs on the causes of IBD, assessed by qualitative thematic analysis.
Results: In 649 adults (62% female; median age 38 years, 63% Crohn’s disease), 45% had clinically active IBD, which was associated with negative illness perceptions, particularly IBD’s impact on their lives (consequence: aOR 4.8, 95% CI 3.2-7.4), lower treatment effectiveness (treatment control: aOR 2.3, 95% CI 1.4-3.0), more severe symptoms from IBD (identity: aOR 9.3, 95% CI 5.5-15.9), more concern about IBD (concern: aOR 3.8, 95% CI 2.5-5.8), and feeling angry, scared, upset or depressed because of IBD (negative emotional response: aOR 3.4, 95% CI 2.2-5.4) (all p< .001 on univariate and multivariable analyses; Table 1).
On thematic analysis, patients most often believed that IBD was caused by stress (25% of all themes), diet (21%), genetics (18%), lifestyle (7%, including sleep, exercise, substance use), or was a secondary effect of another illness or medical event (5%, including consequence of another illness, medication, or pregnancy).
Discussion: Negative illness perceptions are associated with clinically active disease in adults with inflammatory bowel diseases. Psychosocial interventions that target negative illness perceptions, such as cognitive behavioral therapy and patient-centered information on the etiology of IBD, may be an effective adjunct therapy in adults with active IBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
David Bickford, MD1, Emily Sheng, BA1, Melissa G. Hunt, PhD2, Sara N. Horst, MD3, Samir A. Shah, MD4, Sumona Saha, MD, MS5, Sasha Taleban, MD6, Lily Brown, PhD1, Kanika Malani, BS7, Megan Lutz, MD8, Hannah Fiske, MD9, Robert Kuehnel, PhD1, Brittaney Bonhomme, BA1, Alandra Weaver, MPH10, Millie D. Long, MD, MPH11, Raymond Cross, MD12, James Lewis, MD, MSCE13, Chung Sang Tse, MD2. P2590 - Negative Illness Perceptions are Associated With Clinical Disease Activity in Adult Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Hospital of the University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI; 5University of Wisconsin Hospitals and Clinics, Madison, WI; 6University of Arizona, Tucson, AZ; 7The Warren Alpert Medical School of Brown University, Providence, RI; 8University of Wisconsin-Madison, Madison, WI; 9Brown University / Rhode Island Hospital, Providence, RI; 10Crohn's and Colitis Foundation, New York, NY; 11Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 12University of Maryland School of Medicine, Baltimore, MD; 13Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA
Introduction: Illness perceptions are emotional and cognitive beliefs that may influence a person’s psychological coping, health behavior, and chronic disease course. However, there is a knowledge gap for how illness perceptions are associated with disease activity in adults with inflammatory bowel diseases (IBD).
Methods: We conducted a mixed-methods survey study on adults with IBD from five geographically diverse gastroenterology practices participating in the Crohn’s and Colitis Foundation’s Clinical Research Alliance’s ADEPT Trial (NCT05635292). We used multivariable logistic regression models to assess for associations between negative illness perceptions and clinical disease activity (2-item patient-reported outcome, PRO-2), adjusted for age, gender, and IBD subtype. The Brief Illness Perception Questionnaire (BIPQ) assesses eight cognitive and emotional representations of IBD (0-5 Likert scale, cut points at >75th interquartile for negative illness perceptions, with reversed coding for positively worded items) and an open-ended question on patients’ personal beliefs on the causes of IBD, assessed by qualitative thematic analysis.
Results: In 649 adults (62% female; median age 38 years, 63% Crohn’s disease), 45% had clinically active IBD, which was associated with negative illness perceptions, particularly IBD’s impact on their lives (consequence: aOR 4.8, 95% CI 3.2-7.4), lower treatment effectiveness (treatment control: aOR 2.3, 95% CI 1.4-3.0), more severe symptoms from IBD (identity: aOR 9.3, 95% CI 5.5-15.9), more concern about IBD (concern: aOR 3.8, 95% CI 2.5-5.8), and feeling angry, scared, upset or depressed because of IBD (negative emotional response: aOR 3.4, 95% CI 2.2-5.4) (all p< .001 on univariate and multivariable analyses; Table 1).
On thematic analysis, patients most often believed that IBD was caused by stress (25% of all themes), diet (21%), genetics (18%), lifestyle (7%, including sleep, exercise, substance use), or was a secondary effect of another illness or medical event (5%, including consequence of another illness, medication, or pregnancy).
Discussion: Negative illness perceptions are associated with clinically active disease in adults with inflammatory bowel diseases. Psychosocial interventions that target negative illness perceptions, such as cognitive behavioral therapy and patient-centered information on the etiology of IBD, may be an effective adjunct therapy in adults with active IBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
David Bickford indicated no relevant financial relationships.
Emily Sheng indicated no relevant financial relationships.
Melissa Hunt indicated no relevant financial relationships.
Sara Horst: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Takeda – Consultant.
Samir Shah: Roche Information Systems – Consultant.
Sumona Saha indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Advisory Committee/Board Member. Bristol Myers Squibb – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Lily Brown indicated no relevant financial relationships.
Kanika Malani indicated no relevant financial relationships.
Megan Lutz indicated no relevant financial relationships.
Hannah Fiske indicated no relevant financial relationships.
Robert Kuehnel indicated no relevant financial relationships.
Brittaney Bonhomme indicated no relevant financial relationships.
Alandra Weaver indicated no relevant financial relationships.
Millie Long: AbbVie – Consultant. Bristol-Myers Squibb – Consultant. Eli Lilly – Consultant, Grant/Research Support. Intercept – Consultant. Janssen – Consultant. Pfizer Inc – Consultant, Grant/Research Support. Prometheus – Consultant. Roche – Consultant. Roivant – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant.
Raymond Cross: Abbvie – Advisory Committee/Board Member, Consultant. Adiso – Advisory Committee/Board Member, Consultant. BMS – Advisory Committee/Board Member, Consultant. Fresenius Kabi – Advisory Committee/Board Member, Consultant. Fzata – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Magellan Health – Advisory Committee/Board Member, Consultant. Option Care – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Pharmacosmos – Advisory Committee/Board Member, Consultant. Samsung Bioepis – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. Sebela – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant.
James Lewis: AbbVie – Consultant, Grant/Research Support. Amgen – Advisory Committee/Board Member. Arena Pharmaceuticals – Advisory Committee/Board Member. Bridge Biotherapeutics – Consultant. Celgene/BMS – Consultant. Entasis Therapeutics – Consultant. Galapagos – Advisory Committee/Board Member. Gilead – Advisory Committee/Board Member. Janssen – Consultant, Grant/Research Support. Merck – Consultant. Nestle Health Science – Grant/Research Support. Pfizer – Advisory Committee/Board Member. Protagonist Therapeutics – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member. Scipher Medicine – Consultant. Takeda – Grant/Research Support.
Chung Sang Tse indicated no relevant financial relationships.
David Bickford, MD1, Emily Sheng, BA1, Melissa G. Hunt, PhD2, Sara N. Horst, MD3, Samir A. Shah, MD4, Sumona Saha, MD, MS5, Sasha Taleban, MD6, Lily Brown, PhD1, Kanika Malani, BS7, Megan Lutz, MD8, Hannah Fiske, MD9, Robert Kuehnel, PhD1, Brittaney Bonhomme, BA1, Alandra Weaver, MPH10, Millie D. Long, MD, MPH11, Raymond Cross, MD12, James Lewis, MD, MSCE13, Chung Sang Tse, MD2. P2590 - Negative Illness Perceptions are Associated With Clinical Disease Activity in Adult Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
