Monday Poster Session
Category: GI Bleeding
P2514 - Unveiling the Uncommon: Gastrointestinal Mucormycosis Unmasked by Gastrointestinal Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yash Kanani, MBBS, MD
Deenanath Mangeshkar Hospital and Research Center
Pune, Maharashtra, India
Presenting Author(s)
Yash Kanani, MBBS, MD, Chetan Oswal, MBBS, MD, Sanjana Bhagwat, MBBS, MD, Chaitanya Kumbhar, MBBS, MD, Amol Bapaye, MBBS, Harshal Gadhikar, MBBS, MD, DM
Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India
Introduction: Mucormycosis, a life-threatening multiple-system fungal infection caused by mucormycetes, of the Mucorales order. Gastrointestinal (GI) mucormycosis cases are on rise even in immunocompetent individuals.Stomach involvement is most common followed by large and small intestine.Here we present a short 3 case series of GI mucormycosis presented as GI bleed.
Case Description/Methods: Case 1
A 34-yr female admitted with fever and recurrent seizures, unresponsive to multiple anti-epileptic drugs. Initial brain scans were normal, blood tests positivie for rickettsial PCR.Seizures persisted, leading to ventilator support and after three cycles of plasma exchange, the patient developed GI bleed with fall in Haemoglobin(Hb). On gastroscopy large, irregular, sloughed ulcer in the stomach, later confirmed as mucormycosis upon biopsy.
Case 2
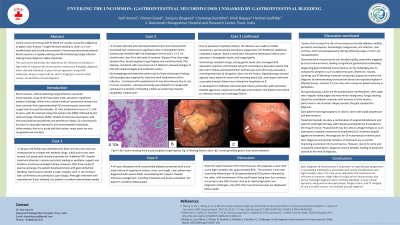
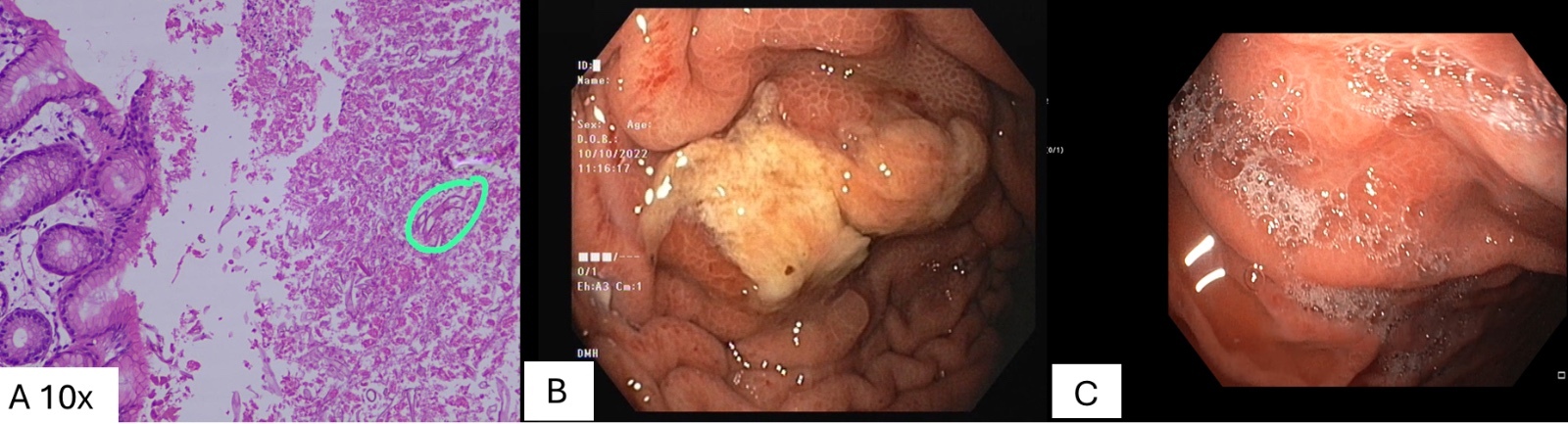
"A 53-yr male with decompensated chronic liver disease(CLD) presented with melena and drop in Hblevels. Gastroscopy(Figure B ) revealed irregular 3 cm sloughed ulcer in the body of stomach. Biopsy of the ulcer edge showed thick, broad aseptate fungal hyphae(Figure A) and on PAS staining consistent with mucormycosis.Otolaryngology evaluation negative for head and neck involvement. Treated with amphotericin-B and later isavuconazole for 6 weeks. Follow-up endoscopy(Figure C) showed completely healed ulcer.
Case 3
A 44-yr male with uncontrolled diabetes,1 week history of respiratory distress, fever, and cough.Diagnosed with severe ARDS likely viral etiology, requiring NIV support subsequently intubation and prone ventilation.Later initiated on venovenous extracorporeal membrane oxygenation. 1 week later, the patient had GI bleed with fall in Hb.Gastroscopy showed large irregular ulcer in body and fundus with sloughed base. Sigmoidoscopy showed sigmoid colon extensive ulcers with overlying blood clot, and biopsy confirmed mucorales invasion.
Discussion: GI mucormycosis evolves rapidly and have high mortality rate. Potentially triggered by stress-induced ulcers, leading to gastrointestinal bleeding. On endoscopy ulcers are often large with irregular rolled edges and sloughed base. Edge biopsy shows broad aseptate hyphae. Contrast CT scan may aid in ruling out bowel ischemia. This case series highlights importance of pursuing histologic diagnosis in patient with G.I bleed in patients with high risks features for Mucormycosis. Early diagnosis and prompt treatment are crucial for improving outcomes in GI mucormycosis.
Disclosures:
Yash Kanani, MBBS, MD, Chetan Oswal, MBBS, MD, Sanjana Bhagwat, MBBS, MD, Chaitanya Kumbhar, MBBS, MD, Amol Bapaye, MBBS, Harshal Gadhikar, MBBS, MD, DM. P2514 - Unveiling the Uncommon: Gastrointestinal Mucormycosis Unmasked by Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India
Introduction: Mucormycosis, a life-threatening multiple-system fungal infection caused by mucormycetes, of the Mucorales order. Gastrointestinal (GI) mucormycosis cases are on rise even in immunocompetent individuals.Stomach involvement is most common followed by large and small intestine.Here we present a short 3 case series of GI mucormycosis presented as GI bleed.
Case Description/Methods: Case 1
A 34-yr female admitted with fever and recurrent seizures, unresponsive to multiple anti-epileptic drugs. Initial brain scans were normal, blood tests positivie for rickettsial PCR.Seizures persisted, leading to ventilator support and after three cycles of plasma exchange, the patient developed GI bleed with fall in Haemoglobin(Hb). On gastroscopy large, irregular, sloughed ulcer in the stomach, later confirmed as mucormycosis upon biopsy.
Case 2
"A 53-yr male with decompensated chronic liver disease(CLD) presented with melena and drop in Hblevels. Gastroscopy(Figure B ) revealed irregular 3 cm sloughed ulcer in the body of stomach. Biopsy of the ulcer edge showed thick, broad aseptate fungal hyphae(Figure A) and on PAS staining consistent with mucormycosis.Otolaryngology evaluation negative for head and neck involvement. Treated with amphotericin-B and later isavuconazole for 6 weeks. Follow-up endoscopy(Figure C) showed completely healed ulcer.
Case 3
A 44-yr male with uncontrolled diabetes,1 week history of respiratory distress, fever, and cough.Diagnosed with severe ARDS likely viral etiology, requiring NIV support subsequently intubation and prone ventilation.Later initiated on venovenous extracorporeal membrane oxygenation. 1 week later, the patient had GI bleed with fall in Hb.Gastroscopy showed large irregular ulcer in body and fundus with sloughed base. Sigmoidoscopy showed sigmoid colon extensive ulcers with overlying blood clot, and biopsy confirmed mucorales invasion.
Discussion: GI mucormycosis evolves rapidly and have high mortality rate. Potentially triggered by stress-induced ulcers, leading to gastrointestinal bleeding. On endoscopy ulcers are often large with irregular rolled edges and sloughed base. Edge biopsy shows broad aseptate hyphae. Contrast CT scan may aid in ruling out bowel ischemia. This case series highlights importance of pursuing histologic diagnosis in patient with G.I bleed in patients with high risks features for Mucormycosis. Early diagnosis and prompt treatment are crucial for improving outcomes in GI mucormycosis.
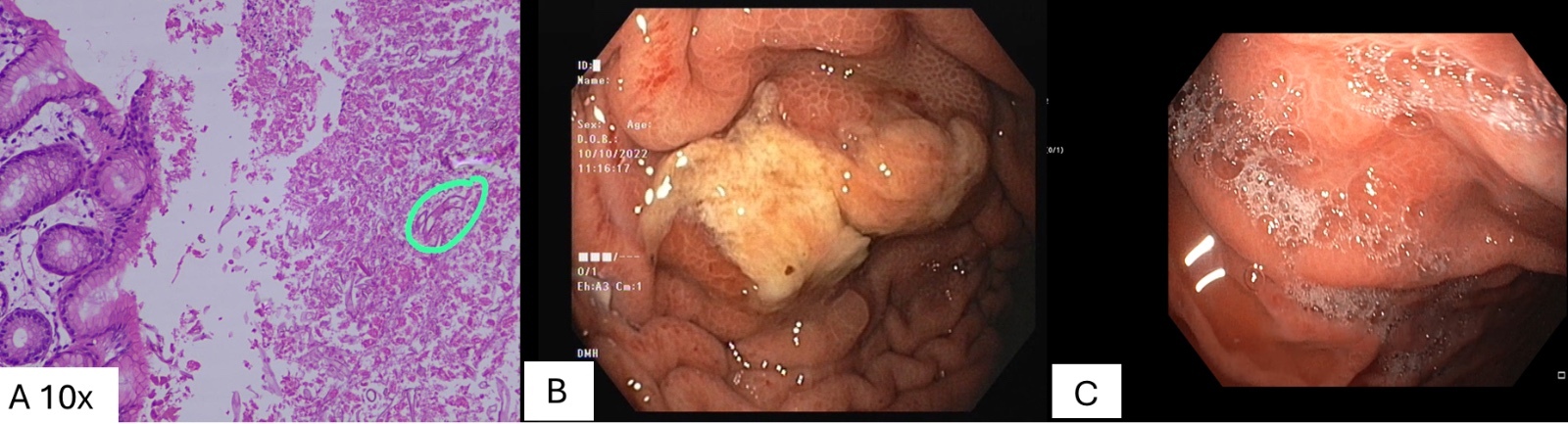
Figure: Fig A H & E stains showing thick broad aseptate fungal hyphae
Fig. B Showing Gastric ulcer
Fig C showing healed gastric ulcer post treatment.
Fig. B Showing Gastric ulcer
Fig C showing healed gastric ulcer post treatment.
Disclosures:
Yash Kanani indicated no relevant financial relationships.
Chetan Oswal indicated no relevant financial relationships.
Sanjana Bhagwat indicated no relevant financial relationships.
Chaitanya Kumbhar indicated no relevant financial relationships.
Amol Bapaye indicated no relevant financial relationships.
Harshal Gadhikar indicated no relevant financial relationships.
Yash Kanani, MBBS, MD, Chetan Oswal, MBBS, MD, Sanjana Bhagwat, MBBS, MD, Chaitanya Kumbhar, MBBS, MD, Amol Bapaye, MBBS, Harshal Gadhikar, MBBS, MD, DM. P2514 - Unveiling the Uncommon: Gastrointestinal Mucormycosis Unmasked by Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
