Monday Poster Session
Category: GI Bleeding
P2523 - A Tale of Two Vessels: Giant Duodenal AVM Successfully Managed by Embolization
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mikayla S. Hennen, DO
University of Louisville
Louisville, KY
Presenting Author(s)
Mikayla S. Hennen, DO, Navroop Nagra, MD, Brett Rossow, MD
University of Louisville, Louisville, KY
Introduction: Arteriovenous malformations (AVMs) are abnormal connections between the arteries and veins without capillaries. They comprise 5% of non-variceal upper gastrointestinal (GI) bleeding. Typically, these are small lesions which cause slow blood loss, massive GI bleeding is uncommon. Herein, we describe a case of severe GI bleeding from a large duodenal AVM causing near syncopal episode.
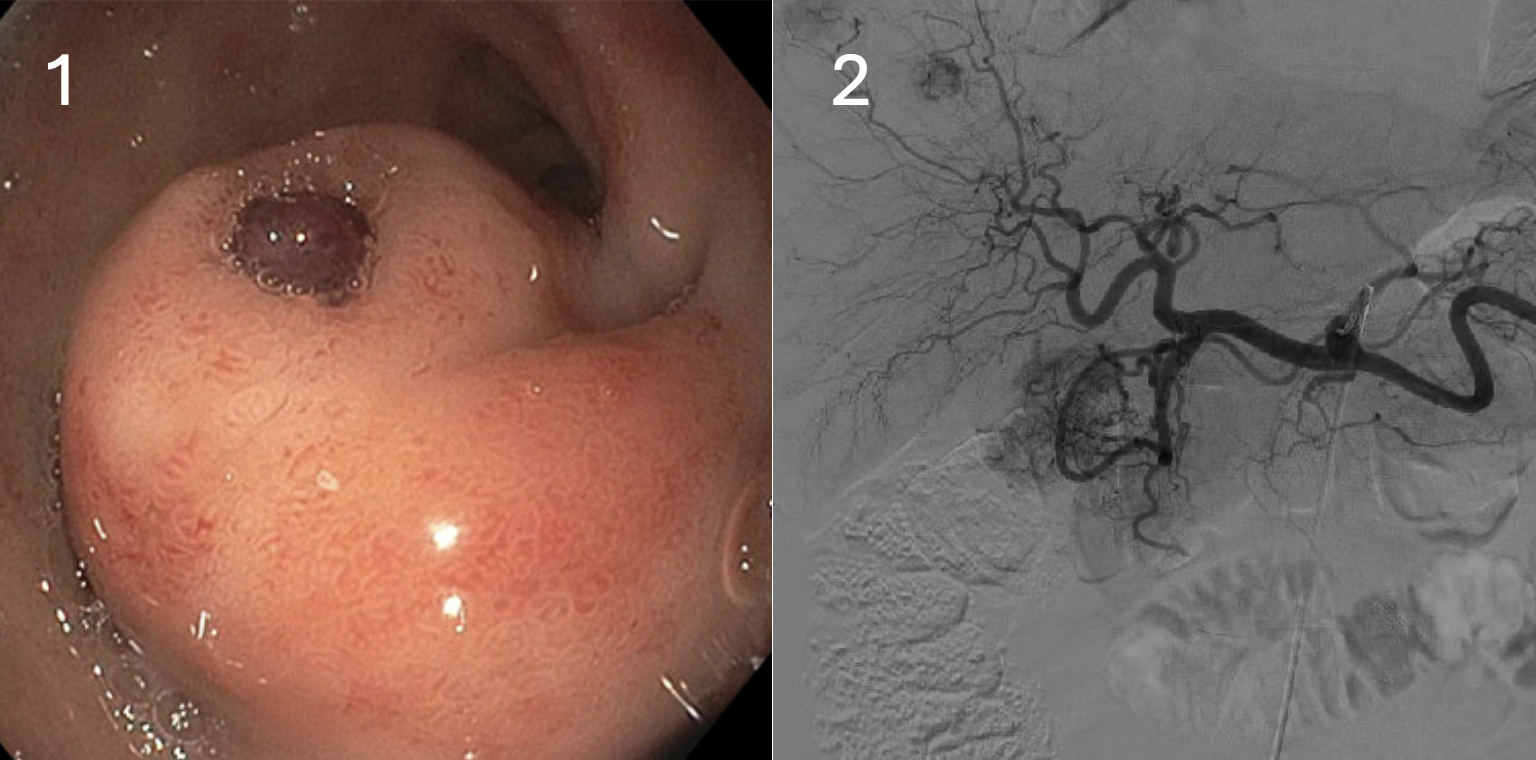
Case Description/Methods: A 59-year-old man presented with two days of melena and one episode of hematemesis with a near-syncope episode. He was initially hypotensive but responded well to fluids. CT Angiography revealed a heterogenous and hyper-vascular mass measuring 3.2 cm along the first and second portion of duodenum, no active extravasation was seen. Upper endoscopy demonstrated a submucosal appearing lesion with an adherent clot in the first portion of the duodenum (Figure 1). There was no active bleeding, however upon placing a hemostatic clip, active bleeding was visualized. Four hemoclips were placed and epinephrine was injected, the combination of which resolved the bleeding. Considering the size of the lesion and the amount of bleeding it caused, the patient underwent a gastroduodenal arteriogram with interventional radiology which revealed that the hyper-vascular duodenal lesion was an AVM with at least two supplying arteries arising from the gastroduodenal artery (Figure 2). The lesion was successfully embolized with no evidence of further bleeding, and the patient was safely discharged home with outpatient follow-up.
Discussion: AVMs in the duodenum makeup approximately 2.3% of all GI tract AVMs. Presentation of these vascular lesions can range from asymptomatic iron deficiency anemia to hemorrhagic shock. Argon plasma coagulation (APC) ablation, band ligation, hemoclips and injection sclerotherapy are various endoscopically available techniques to treat these AVMs. The choice of management relies heavily on patient presentation and hemodynamic stability. The AVM in our patient is unique as it was large with two arterial feeders which caused massive bleeding. IR embolization is the preferred treatment modality in these cases as there is high risk of recurrent bleeding with endoscopic intervention alone.
Disclosures:
Mikayla S. Hennen, DO, Navroop Nagra, MD, Brett Rossow, MD. P2523 - A Tale of Two Vessels: Giant Duodenal AVM Successfully Managed by Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Louisville, Louisville, KY
Introduction: Arteriovenous malformations (AVMs) are abnormal connections between the arteries and veins without capillaries. They comprise 5% of non-variceal upper gastrointestinal (GI) bleeding. Typically, these are small lesions which cause slow blood loss, massive GI bleeding is uncommon. Herein, we describe a case of severe GI bleeding from a large duodenal AVM causing near syncopal episode.
Case Description/Methods: A 59-year-old man presented with two days of melena and one episode of hematemesis with a near-syncope episode. He was initially hypotensive but responded well to fluids. CT Angiography revealed a heterogenous and hyper-vascular mass measuring 3.2 cm along the first and second portion of duodenum, no active extravasation was seen. Upper endoscopy demonstrated a submucosal appearing lesion with an adherent clot in the first portion of the duodenum (Figure 1). There was no active bleeding, however upon placing a hemostatic clip, active bleeding was visualized. Four hemoclips were placed and epinephrine was injected, the combination of which resolved the bleeding. Considering the size of the lesion and the amount of bleeding it caused, the patient underwent a gastroduodenal arteriogram with interventional radiology which revealed that the hyper-vascular duodenal lesion was an AVM with at least two supplying arteries arising from the gastroduodenal artery (Figure 2). The lesion was successfully embolized with no evidence of further bleeding, and the patient was safely discharged home with outpatient follow-up.
Discussion: AVMs in the duodenum makeup approximately 2.3% of all GI tract AVMs. Presentation of these vascular lesions can range from asymptomatic iron deficiency anemia to hemorrhagic shock. Argon plasma coagulation (APC) ablation, band ligation, hemoclips and injection sclerotherapy are various endoscopically available techniques to treat these AVMs. The choice of management relies heavily on patient presentation and hemodynamic stability. The AVM in our patient is unique as it was large with two arterial feeders which caused massive bleeding. IR embolization is the preferred treatment modality in these cases as there is high risk of recurrent bleeding with endoscopic intervention alone.
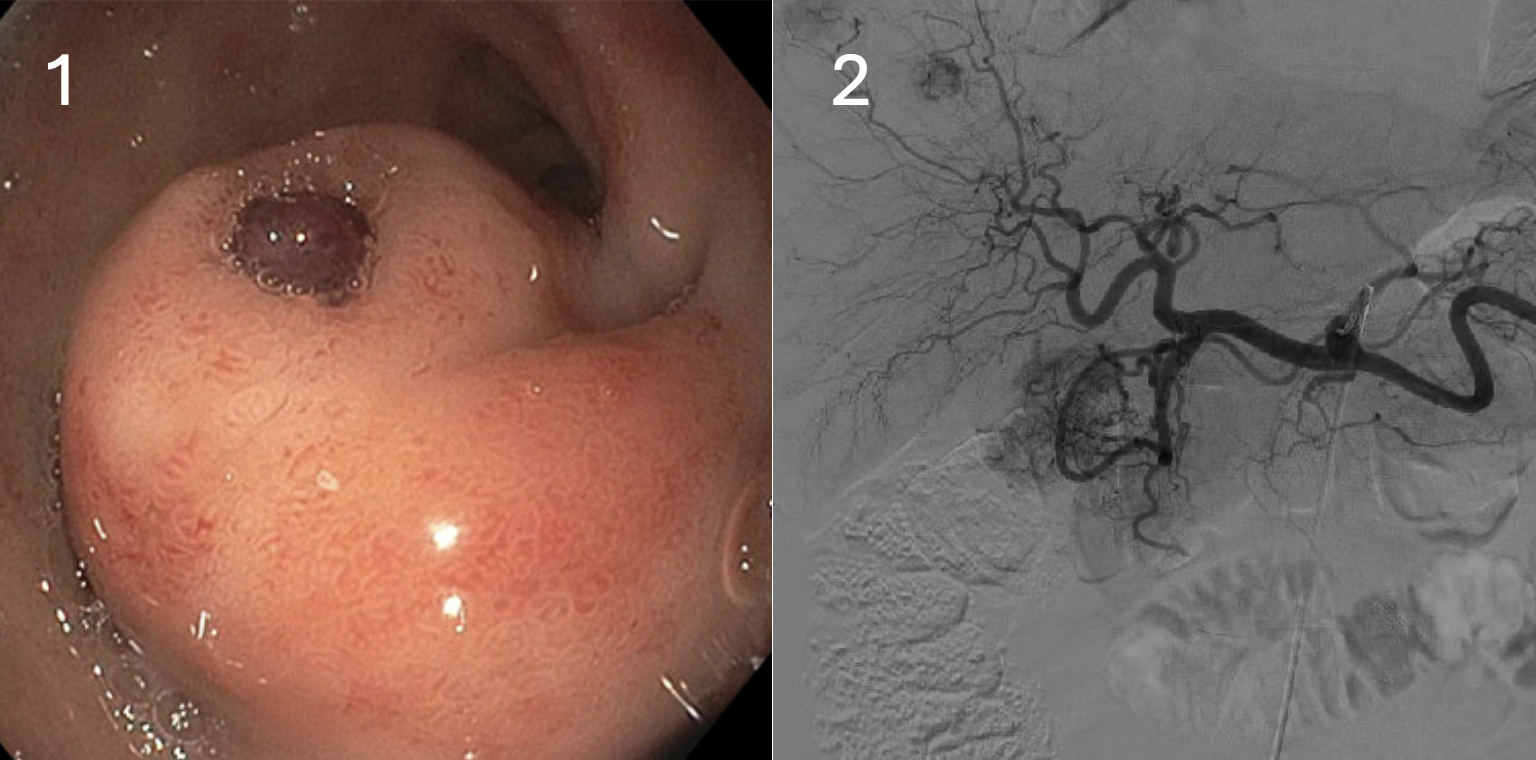
Figure: Figure 1: Submucosal lesion with an adherent clot in the first portion of the duodenum
Figure 2: Gastroduodenal arteriogram demonstrating a hypervascular small bowel AVM
Figure 2: Gastroduodenal arteriogram demonstrating a hypervascular small bowel AVM
Disclosures:
Mikayla Hennen indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Brett Rossow indicated no relevant financial relationships.
Mikayla S. Hennen, DO, Navroop Nagra, MD, Brett Rossow, MD. P2523 - A Tale of Two Vessels: Giant Duodenal AVM Successfully Managed by Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
