Monday Poster Session
Category: GI Bleeding
P2442 - Relationship Between the Glasgow Blatchford Score and Findings on Esophagogastroduodenoscopy in an Urban Healthcare System
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Joseph O. Atarere, MD, MPH
MedStar Union Memorial Hospital
Baltimore, MD
Presenting Author(s)
Joseph O. Atarere, MD, MPH1, Thilini Delungahawatta, MD2, Boniface Mensah, MBChB, MPH1, Ramya Vasireddy, MBBS1, Sarah Rimm, MD3, Jose Mari Parungao, MD2, David Weisman, DO1, Christopher Haas, MD, PhD2, Haider A. Naqvi, MD3, Dana Sloane, MD3
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Health, Baltimore, MD; 3MedStar Franklin Square Medical Center, Rossville, MD
Introduction: The Glasgow Blatchford Score (GBS) is one of the most widely used scoring systems for risk stratifying patients with upper gastrointestinal bleeding (UGIB) for admission versus outpatient management. Among those admitted, computed tomography angiography (CTA) is the radiological test of choice for evaluating hemodynamically stable active GIB. Those with active GIB on CTA are managed either by urgent embolization or esophagogastroduodenoscopy (EGD). There are no consensus guidelines for managing patients with a negative CTA and the GBS has not been validated for stratifying patients with negative CTA for inpatient EGD. The aims of this study were to (1) compare the GBS with ulcer severity on EGD and (2) determine if the relationship differed by CTA findings.
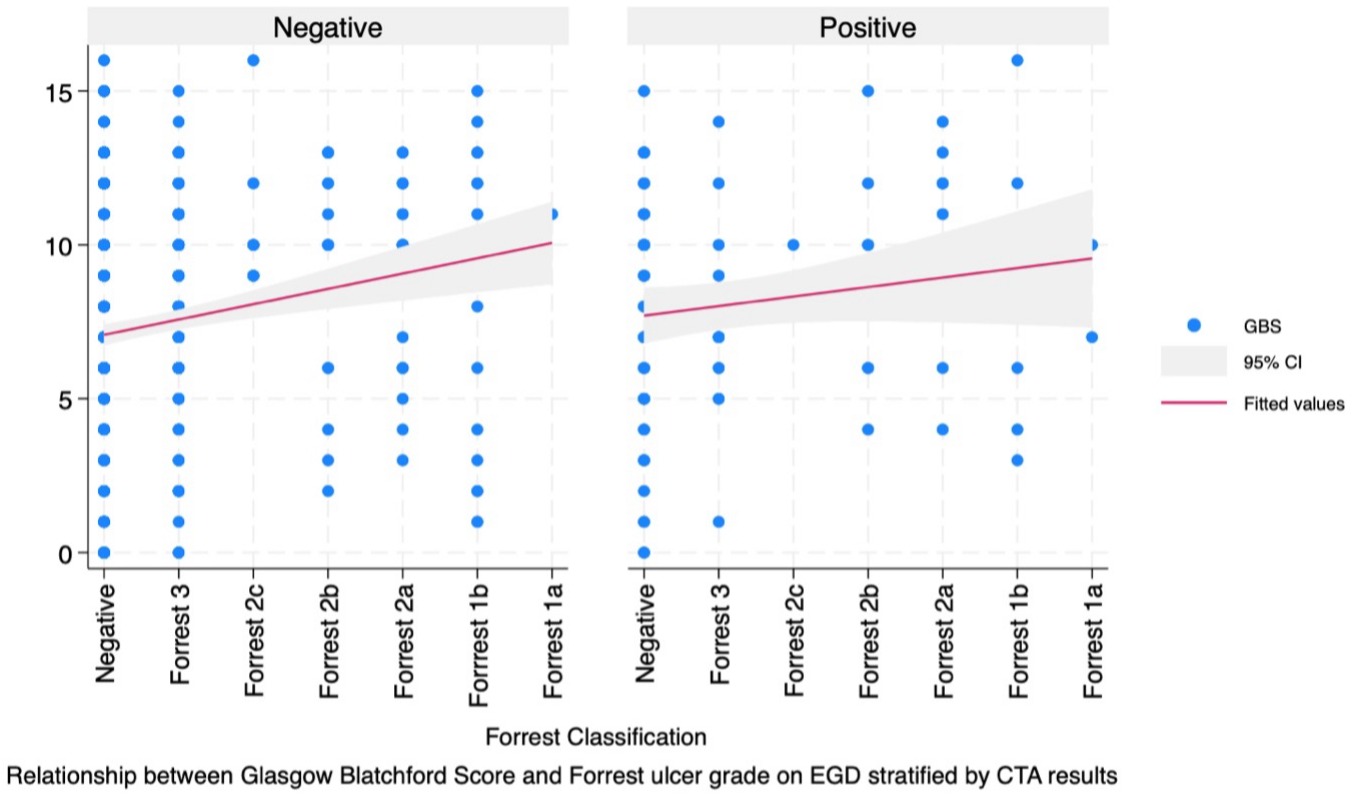
Methods: We used data from patients in an urban healthcare system who either presented with or developed UGIB during admission and received a CTA between January 1st, 2018, and September 1st, 2022. We included patients who underwent inpatient EGD after CTA. The outcome of interest was the grade of ulcer on EGD (Forrest III, IIc, IIb, IIa, Ib or Ia) and the primary predictor was the GBS. We compared the GBS with ulcer grade on EGD using a two-way scatter plot stratified by CTA findings (positive or negative). Furthermore, we evaluated the strength of this relationship using a Spearman’s test.
Results: A total of 677 patients met inclusion criteria for this study of which 91 (13.4%) had positive results on CTA. Most (89.5%) of the participants had a GBS of at least 2. Almost a third of patients (219; 32.3%) had an ulcer on EGD; 128 (18.9%) were Forrest III, 64 (9.5%) were Forrest II, and 27 (4.0%) were Forrest I. There was a weakly positive relationship between GBS and ulcer grade on EGD among patients with negative CTA results (Spearman’s rho= 0.195; p< 0.001). However, among those with positive CTA results, this relationship was not significant (Spearman’s rho= 0.107; p= 0.314) (Fig. 1).
Discussion: The GBS is widely used in guiding decisions for outpatient versus inpatient management of UGIB. Our findings support its use in guiding decisions for inpatient EGD among patients with negative CTA. Further studies will be needed to externally validate our findings and determine the optimum GBS cutoff for inpatient EGD.
Disclosures:
Joseph O. Atarere, MD, MPH1, Thilini Delungahawatta, MD2, Boniface Mensah, MBChB, MPH1, Ramya Vasireddy, MBBS1, Sarah Rimm, MD3, Jose Mari Parungao, MD2, David Weisman, DO1, Christopher Haas, MD, PhD2, Haider A. Naqvi, MD3, Dana Sloane, MD3. P2442 - Relationship Between the Glasgow Blatchford Score and Findings on Esophagogastroduodenoscopy in an Urban Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Health, Baltimore, MD; 3MedStar Franklin Square Medical Center, Rossville, MD
Introduction: The Glasgow Blatchford Score (GBS) is one of the most widely used scoring systems for risk stratifying patients with upper gastrointestinal bleeding (UGIB) for admission versus outpatient management. Among those admitted, computed tomography angiography (CTA) is the radiological test of choice for evaluating hemodynamically stable active GIB. Those with active GIB on CTA are managed either by urgent embolization or esophagogastroduodenoscopy (EGD). There are no consensus guidelines for managing patients with a negative CTA and the GBS has not been validated for stratifying patients with negative CTA for inpatient EGD. The aims of this study were to (1) compare the GBS with ulcer severity on EGD and (2) determine if the relationship differed by CTA findings.
Methods: We used data from patients in an urban healthcare system who either presented with or developed UGIB during admission and received a CTA between January 1st, 2018, and September 1st, 2022. We included patients who underwent inpatient EGD after CTA. The outcome of interest was the grade of ulcer on EGD (Forrest III, IIc, IIb, IIa, Ib or Ia) and the primary predictor was the GBS. We compared the GBS with ulcer grade on EGD using a two-way scatter plot stratified by CTA findings (positive or negative). Furthermore, we evaluated the strength of this relationship using a Spearman’s test.
Results: A total of 677 patients met inclusion criteria for this study of which 91 (13.4%) had positive results on CTA. Most (89.5%) of the participants had a GBS of at least 2. Almost a third of patients (219; 32.3%) had an ulcer on EGD; 128 (18.9%) were Forrest III, 64 (9.5%) were Forrest II, and 27 (4.0%) were Forrest I. There was a weakly positive relationship between GBS and ulcer grade on EGD among patients with negative CTA results (Spearman’s rho= 0.195; p< 0.001). However, among those with positive CTA results, this relationship was not significant (Spearman’s rho= 0.107; p= 0.314) (Fig. 1).
Discussion: The GBS is widely used in guiding decisions for outpatient versus inpatient management of UGIB. Our findings support its use in guiding decisions for inpatient EGD among patients with negative CTA. Further studies will be needed to externally validate our findings and determine the optimum GBS cutoff for inpatient EGD.
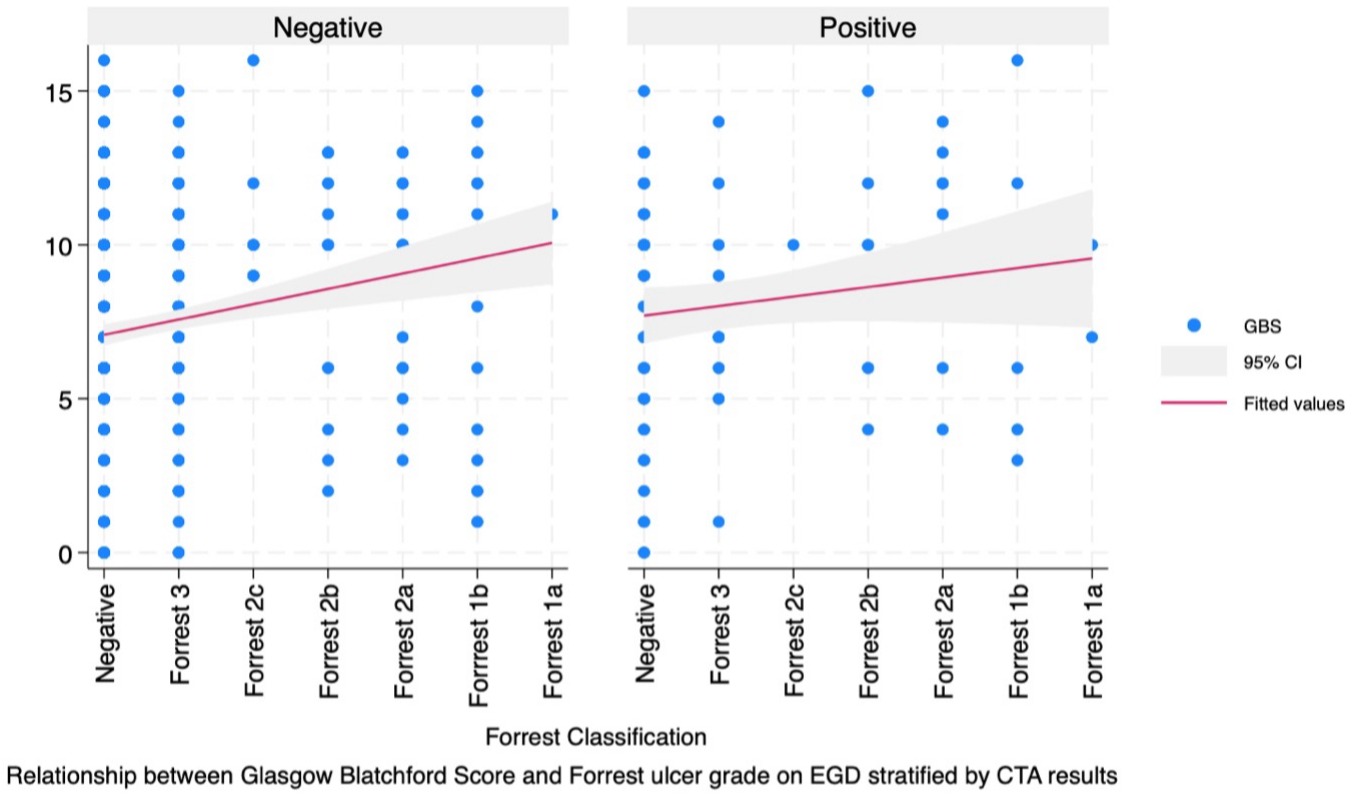
Figure: Figure 1: Two-way scatter plot with fitted line and 95% confidence interval showing the relationship between Glasgow Blatchford Score (GBS) and Forrest grade on EGD stratified by CTA findings.
Disclosures:
Joseph Atarere indicated no relevant financial relationships.
Thilini Delungahawatta indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Sarah Rimm indicated no relevant financial relationships.
Jose Mari Parungao indicated no relevant financial relationships.
David Weisman indicated no relevant financial relationships.
Christopher Haas indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Dana Sloane indicated no relevant financial relationships.
Joseph O. Atarere, MD, MPH1, Thilini Delungahawatta, MD2, Boniface Mensah, MBChB, MPH1, Ramya Vasireddy, MBBS1, Sarah Rimm, MD3, Jose Mari Parungao, MD2, David Weisman, DO1, Christopher Haas, MD, PhD2, Haider A. Naqvi, MD3, Dana Sloane, MD3. P2442 - Relationship Between the Glasgow Blatchford Score and Findings on Esophagogastroduodenoscopy in an Urban Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
