Monday Poster Session
Category: GI Bleeding
P2456 - July Effect on Clinical Outcomes of Patients Presenting With Lower Gastrointestinal Bleeding at Teaching Hospitals in the United States
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Eugene Annor, MD, MPH
University of Illinois College of Medicine
Morton, IL
Presenting Author(s)
Eugene Annor, MD, MPH1, Joseph Atarere, MD, MPH2, Chima Amadi, MD, MBA3, Toni M. Jackson, DO4, Oluwatayo J. Awolumate, MD5, Adedeji Adenusi, MD, MPH6, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG7
1University of Illinois College of Medicine, Morton, IL; 2MedStar Union Memorial Hospital, Baltimore, MD; 3Morehouse School of Medicine, Atlanta, GA; 4Morehouse School of Medicine, Far Rockaway, NY; 5Howard University Hospital, Washington, DC; 6One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 7Loyola University Medical Center, Maywood, IL
Introduction: “July effect” is a term coined for an increase in morbidity and mortality associated with cohorts of new trainees starting at teaching hospitals in July. This phenomenon has been seen in numerous conditions, but it is yet to be explored in lower gastrointestinal bleeding (LGIB). LGIB accounts for 20% to 30% of patients admitted for major GI bleeding, with mortality rates ranging from 2% to 4%. This study aims to evaluate the “July effect” on clinical outcomes of patients presenting with LGIB at teaching hospitals in the US from 2016 to 2020.
Methods: Retrospective cohort study using data from the Nationwide Inpatient Sample (2016 to 2020). The outcomes of interest were inpatient mortality, hospital length of stay (LOS), and delay in early colonoscopy, defined as a time to colonoscopy of >24 hours from admission. The primary variable of interest was the month of admission, classified as pre-July (May and June) and July effect (July and August). We evaluated the impact of the month of admission on study outcomes using survey-weighted multivariable logistic and Poisson regression models.
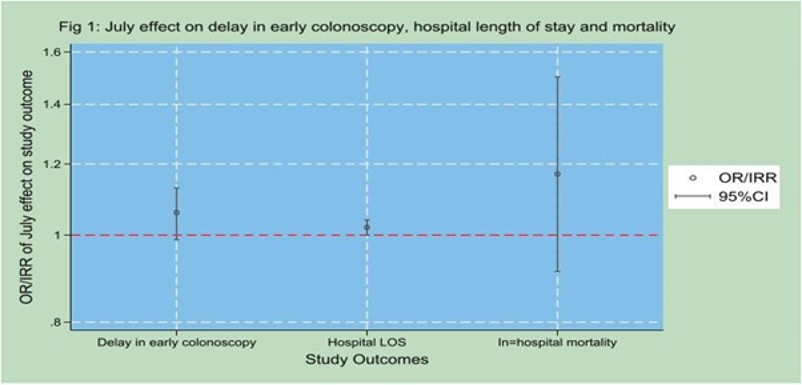
Results: A total of 27,425 admissions met the inclusion criteria, of which 13,746 (50.1%) were admitted in May and June, while 13,679 (49.9%) were admitted in July and August. (Fig. 1). Less than two-thirds (59.2%) of the admissions for LGIB received a colonoscopy during their hospital stay. Among the 15,708 patients who underwent colonoscopy within seven days of admission, 40.8% received it early (within 24 hours). The overall mean hospital LOS was 4.4 days, while the in-hospital mortality rate was 1%. We found no significant July effect on delay in early colonoscopy [adjusted odds ratio (aOR) 1.06, 95% CI (0.99, 1.13)], hospital LOS [adjusted incidence rate ratio (aIRR) 1.02, 95% CI (1.00, 1.04)] or in-hospital mortality [aOR 1.17, 95% CI (0.91, 1.50)].
Discussion: The study found no evidence of the July effect on in-hospital mortality, LOS, or delays in early colonoscopy for patients with LGIB (figure 1). Despite the influx of new trainees in July, the care for LGIB patients in teaching hospitals remains consistent. This suggests that current protocols and supervision have adequately mitigated the risk of adverse outcomes. Future research is needed to explore other factors influencing poor LGIB outcomes and overall patient care in July.
Disclosures:
Eugene Annor, MD, MPH1, Joseph Atarere, MD, MPH2, Chima Amadi, MD, MBA3, Toni M. Jackson, DO4, Oluwatayo J. Awolumate, MD5, Adedeji Adenusi, MD, MPH6, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG7. P2456 - July Effect on Clinical Outcomes of Patients Presenting With Lower Gastrointestinal Bleeding at Teaching Hospitals in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Morton, IL; 2MedStar Union Memorial Hospital, Baltimore, MD; 3Morehouse School of Medicine, Atlanta, GA; 4Morehouse School of Medicine, Far Rockaway, NY; 5Howard University Hospital, Washington, DC; 6One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 7Loyola University Medical Center, Maywood, IL
Introduction: “July effect” is a term coined for an increase in morbidity and mortality associated with cohorts of new trainees starting at teaching hospitals in July. This phenomenon has been seen in numerous conditions, but it is yet to be explored in lower gastrointestinal bleeding (LGIB). LGIB accounts for 20% to 30% of patients admitted for major GI bleeding, with mortality rates ranging from 2% to 4%. This study aims to evaluate the “July effect” on clinical outcomes of patients presenting with LGIB at teaching hospitals in the US from 2016 to 2020.
Methods: Retrospective cohort study using data from the Nationwide Inpatient Sample (2016 to 2020). The outcomes of interest were inpatient mortality, hospital length of stay (LOS), and delay in early colonoscopy, defined as a time to colonoscopy of >24 hours from admission. The primary variable of interest was the month of admission, classified as pre-July (May and June) and July effect (July and August). We evaluated the impact of the month of admission on study outcomes using survey-weighted multivariable logistic and Poisson regression models.
Results: A total of 27,425 admissions met the inclusion criteria, of which 13,746 (50.1%) were admitted in May and June, while 13,679 (49.9%) were admitted in July and August. (Fig. 1). Less than two-thirds (59.2%) of the admissions for LGIB received a colonoscopy during their hospital stay. Among the 15,708 patients who underwent colonoscopy within seven days of admission, 40.8% received it early (within 24 hours). The overall mean hospital LOS was 4.4 days, while the in-hospital mortality rate was 1%. We found no significant July effect on delay in early colonoscopy [adjusted odds ratio (aOR) 1.06, 95% CI (0.99, 1.13)], hospital LOS [adjusted incidence rate ratio (aIRR) 1.02, 95% CI (1.00, 1.04)] or in-hospital mortality [aOR 1.17, 95% CI (0.91, 1.50)].
Discussion: The study found no evidence of the July effect on in-hospital mortality, LOS, or delays in early colonoscopy for patients with LGIB (figure 1). Despite the influx of new trainees in July, the care for LGIB patients in teaching hospitals remains consistent. This suggests that current protocols and supervision have adequately mitigated the risk of adverse outcomes. Future research is needed to explore other factors influencing poor LGIB outcomes and overall patient care in July.
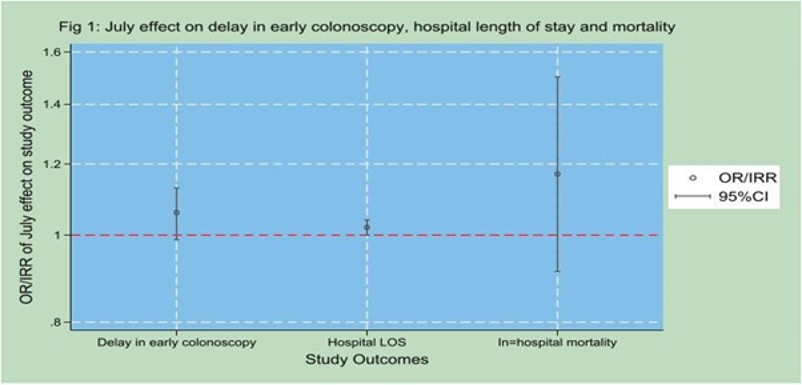
Figure: Figure 1: July effect on delay in early colonoscopy, hospital length of stay and mortality.
Models were adjusted for age, sex, race, health insurance, Charlson Comorbidity Index, illness severity and hospital bed size.
Models were adjusted for age, sex, race, health insurance, Charlson Comorbidity Index, illness severity and hospital bed size.
Disclosures:
Eugene Annor indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Chima Amadi indicated no relevant financial relationships.
Toni Jackson indicated no relevant financial relationships.
Oluwatayo Awolumate indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Ayokunle Abegunde: Ferring Pharmaceuticals – Consultant. Ferring Pharmaceuticals – Consultant.
Eugene Annor, MD, MPH1, Joseph Atarere, MD, MPH2, Chima Amadi, MD, MBA3, Toni M. Jackson, DO4, Oluwatayo J. Awolumate, MD5, Adedeji Adenusi, MD, MPH6, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG7. P2456 - July Effect on Clinical Outcomes of Patients Presenting With Lower Gastrointestinal Bleeding at Teaching Hospitals in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
