Monday Poster Session
Category: General Endoscopy
P2377 - Gastric Biopsy: Deleterious Effects of a Central Needle Within Endoscopy Forceps
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Robert T. Hashimoto, MD
Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center
Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Robert T. Hashimoto, MD1, Theresa Nguyen-Wenker, MD, PhD1, Daniel G. Rosen, MD1, David Y. Graham, MD1, Scott A. Larson, MD, PhD2
1Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 2Baylor College of Medicine, Houston, TX
Introduction: Biopsy forceps vary in jaw size and inclusion of a central needle. Additionally, an endoscopist may obtain a single or multiple bites before withdrawal of endoscopy forceps. Relatively sparse data exist regarding which configurations of forceps and gastric biopsy methods generate optimal histologic quality.
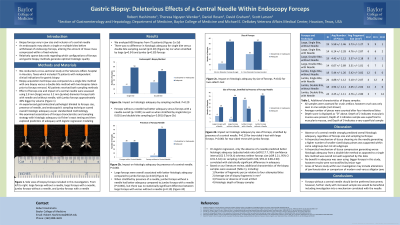
Methods: We conducted a cross-sectional study at the Veterans Affairs hospital in Houston, Texas which included 75 patients with independent clinical indications for gastric biopsy. Biopsy acquisition technique was compared via single bite [SB] method with 1 biopsy versus double bite [DB] method with 2 biopsies prior to withdrawal of forceps. Additionally, effect of forceps size and impact of a central needle was assessed using 2.8 mm [large] versus 3.2 mm [jumbo] diameter forceps both with needle [+N] and without needle [-N], with jumbo forceps approximately 40% bigger by volume (Figure 1). An experienced gastrointestinal pathologist blinded to forceps size, presence of needle, and endoscopist’s sampling technique scored overall histologic adequacy. We examined associations of forceps characteristics and sampling strategy with histologic adequacy via Fisher’s exact testing and then explored predictors of adequacy with logistic regression modeling.
Results: We analyzed 600 biopsies from 75 patients (Table 1). There was no difference in histologic adequacy for SB versus DB sampling overall (p=0.20) nor when stratified by large (p=0.34) and jumbo (p=0.50) forceps. Large forceps were overall associated with better adequacy compared to jumbo (p=0.02). Forceps -N had better adequacy versus forceps +N overall (p< 0.001) as well as when stratified by SB (p< 0.001) and DB sampling (p< 0.001). When stratified by forceps size, jumbo forceps -N had better adequacy compared to +N (P< 0.001), but there was no statistically significant difference between large forceps -N versus +N (p=0.10). On logistic regression, only the absence of a needle predicted better histologic adequacy (adjusted odds ratio [aOR] 17.7, 95% confidence interval [CI] 5.74-54.4) whereas neither forceps size (aOR 2.21, 95% CI 0.91-5.34) nor sampling method (aOR 2.09, 95% CI 0.89-4.90) correlated with statistically significant differences in adequacy.
Discussion: Absence of a needle strongly predicted overall histologic adequacy, regardless of forceps size and sampling technique. Therefore, forceps without a central needle should be the preferred instrument; however, further study with increased sample size would be beneficial.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Robert T. Hashimoto, MD1, Theresa Nguyen-Wenker, MD, PhD1, Daniel G. Rosen, MD1, David Y. Graham, MD1, Scott A. Larson, MD, PhD2. P2377 - Gastric Biopsy: Deleterious Effects of a Central Needle Within Endoscopy Forceps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Robert T. Hashimoto, MD1, Theresa Nguyen-Wenker, MD, PhD1, Daniel G. Rosen, MD1, David Y. Graham, MD1, Scott A. Larson, MD, PhD2
1Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 2Baylor College of Medicine, Houston, TX
Introduction: Biopsy forceps vary in jaw size and inclusion of a central needle. Additionally, an endoscopist may obtain a single or multiple bites before withdrawal of endoscopy forceps. Relatively sparse data exist regarding which configurations of forceps and gastric biopsy methods generate optimal histologic quality.
Methods: We conducted a cross-sectional study at the Veterans Affairs hospital in Houston, Texas which included 75 patients with independent clinical indications for gastric biopsy. Biopsy acquisition technique was compared via single bite [SB] method with 1 biopsy versus double bite [DB] method with 2 biopsies prior to withdrawal of forceps. Additionally, effect of forceps size and impact of a central needle was assessed using 2.8 mm [large] versus 3.2 mm [jumbo] diameter forceps both with needle [+N] and without needle [-N], with jumbo forceps approximately 40% bigger by volume (Figure 1). An experienced gastrointestinal pathologist blinded to forceps size, presence of needle, and endoscopist’s sampling technique scored overall histologic adequacy. We examined associations of forceps characteristics and sampling strategy with histologic adequacy via Fisher’s exact testing and then explored predictors of adequacy with logistic regression modeling.
Results: We analyzed 600 biopsies from 75 patients (Table 1). There was no difference in histologic adequacy for SB versus DB sampling overall (p=0.20) nor when stratified by large (p=0.34) and jumbo (p=0.50) forceps. Large forceps were overall associated with better adequacy compared to jumbo (p=0.02). Forceps -N had better adequacy versus forceps +N overall (p< 0.001) as well as when stratified by SB (p< 0.001) and DB sampling (p< 0.001). When stratified by forceps size, jumbo forceps -N had better adequacy compared to +N (P< 0.001), but there was no statistically significant difference between large forceps -N versus +N (p=0.10). On logistic regression, only the absence of a needle predicted better histologic adequacy (adjusted odds ratio [aOR] 17.7, 95% confidence interval [CI] 5.74-54.4) whereas neither forceps size (aOR 2.21, 95% CI 0.91-5.34) nor sampling method (aOR 2.09, 95% CI 0.89-4.90) correlated with statistically significant differences in adequacy.
Discussion: Absence of a needle strongly predicted overall histologic adequacy, regardless of forceps size and sampling technique. Therefore, forceps without a central needle should be the preferred instrument; however, further study with increased sample size would be beneficial.

Figure: Image 1: Side view of biopsy forceps which were included in this investigation. From left to right: large forceps without a needle, large forceps with a needle, jumbo forceps without a needle, and jumbo forceps with a needle.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Robert Hashimoto indicated no relevant financial relationships.
Theresa Nguyen-Wenker indicated no relevant financial relationships.
Daniel Rosen indicated no relevant financial relationships.
David Graham indicated no relevant financial relationships.
Scott Larson indicated no relevant financial relationships.
Robert T. Hashimoto, MD1, Theresa Nguyen-Wenker, MD, PhD1, Daniel G. Rosen, MD1, David Y. Graham, MD1, Scott A. Larson, MD, PhD2. P2377 - Gastric Biopsy: Deleterious Effects of a Central Needle Within Endoscopy Forceps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

