Monday Poster Session
Category: Esophagus
P2308 - Now You See It, Now You Don't - A Rare Cause of Non-Variceal Upper GI Bleeding in a Cirrhotic Patient: Esophageal Dieulafoy's Lesion
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Annie Shergill, MD
Larkin Community Hospital
Miami Beach, FL
Presenting Author(s)
Annie Shergill, MD1, Hayden Aaron, MD2
1Larkin Community Hospital, Miami Beach, FL; 2West Palm Beach VA Medical Center, West Palm Beach, FL
Introduction: Dieulafoy's Lesion (DL) is an obscure cause of upper GI bleeding (UGIB) wherein an aberrant submucosal vessel erodes into the overlying epithelium, causing hemorrhage. DLs can be located anywhere along the GI tract but are more commonly found in the esophagus & stomach. We present a unique case of a patient with history of decompensated alcoholic cirrhosis, esophageal varices with hematemesis, found to have bleeding DL in the esophagus- an under recognized cause of UGIB in cirrhotics.
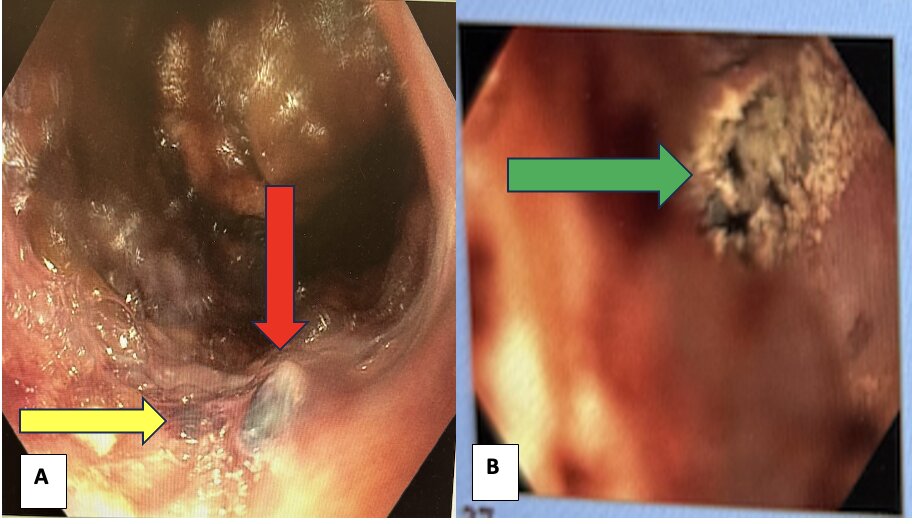
Case Description/Methods: 65-year old male with past medical history of decompensated alcoholic cirrhosis, esophageal varices presented to the ED with nausea, several episodes of vomiting bright red blood. Patient was admitted to the ICU, started on Octreotide & Protonix infusions given concern for variceal hemorrhage and scheduled for an emergent esophagogastroduodenoscopy (EGD). EGD did not show esophageal or gastric varices. However, at 36 cm from incisors, an adherent clot/visible vessel was noted (Figure 1 A) which was challenged & it began to bleed profusely. The lesion was consistent with an esophageal DL which was treated with epinephrine injection & hemospray with cessation of bleeding (Figure 1 B).
Discussion: UGIB is a major cause of morbidity & mortality in cirrhotics. While variceal bleeding constitutes 60-65% of these cases, patients may present with non-variceal UGIB due to portal hypertensive gastropathy, peptic ulcer disease, Mallory Weiss Tears, GAVE & much less commonly- DLs. The incidence of UGIB in cirrhotics secondary to DL can be as low as < 1%. DLs are rarely found in the esophagus, with only a few case reports found & even fewer cases of being reported in cirrhotics presenting with UGIB. The exact etiology & pathophysiology (although portal hypertension causing sheer stress & rupture of submucosal vessels maybe a factor) for DLs remains unknown, making its prevention almost impossible. DL pose a diagnostic and therapeutic challenge due to its obscure & intermittent nature. The aberrant vessel causing bleeding may not be seen unless its actively bleeding. Once identified, modalities such as hemoclips, cautery or hemospray may be used. Our case necessitates keeping a low threshold for this unique entity that is rarely seen in cirrhotics but may actually be under recognized & left untreated. Considering the implications associated with UGIB in cirrhotics, it is prudent that we look for all possible etiologies including ones that we rarely expect to find as in our patient.
Disclosures:
Annie Shergill, MD1, Hayden Aaron, MD2. P2308 - Now You See It, Now You Don't - A Rare Cause of Non-Variceal Upper GI Bleeding in a Cirrhotic Patient: Esophageal Dieulafoy's Lesion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Larkin Community Hospital, Miami Beach, FL; 2West Palm Beach VA Medical Center, West Palm Beach, FL
Introduction: Dieulafoy's Lesion (DL) is an obscure cause of upper GI bleeding (UGIB) wherein an aberrant submucosal vessel erodes into the overlying epithelium, causing hemorrhage. DLs can be located anywhere along the GI tract but are more commonly found in the esophagus & stomach. We present a unique case of a patient with history of decompensated alcoholic cirrhosis, esophageal varices with hematemesis, found to have bleeding DL in the esophagus- an under recognized cause of UGIB in cirrhotics.
Case Description/Methods: 65-year old male with past medical history of decompensated alcoholic cirrhosis, esophageal varices presented to the ED with nausea, several episodes of vomiting bright red blood. Patient was admitted to the ICU, started on Octreotide & Protonix infusions given concern for variceal hemorrhage and scheduled for an emergent esophagogastroduodenoscopy (EGD). EGD did not show esophageal or gastric varices. However, at 36 cm from incisors, an adherent clot/visible vessel was noted (Figure 1 A) which was challenged & it began to bleed profusely. The lesion was consistent with an esophageal DL which was treated with epinephrine injection & hemospray with cessation of bleeding (Figure 1 B).
Discussion: UGIB is a major cause of morbidity & mortality in cirrhotics. While variceal bleeding constitutes 60-65% of these cases, patients may present with non-variceal UGIB due to portal hypertensive gastropathy, peptic ulcer disease, Mallory Weiss Tears, GAVE & much less commonly- DLs. The incidence of UGIB in cirrhotics secondary to DL can be as low as < 1%. DLs are rarely found in the esophagus, with only a few case reports found & even fewer cases of being reported in cirrhotics presenting with UGIB. The exact etiology & pathophysiology (although portal hypertension causing sheer stress & rupture of submucosal vessels maybe a factor) for DLs remains unknown, making its prevention almost impossible. DL pose a diagnostic and therapeutic challenge due to its obscure & intermittent nature. The aberrant vessel causing bleeding may not be seen unless its actively bleeding. Once identified, modalities such as hemoclips, cautery or hemospray may be used. Our case necessitates keeping a low threshold for this unique entity that is rarely seen in cirrhotics but may actually be under recognized & left untreated. Considering the implications associated with UGIB in cirrhotics, it is prudent that we look for all possible etiologies including ones that we rarely expect to find as in our patient.
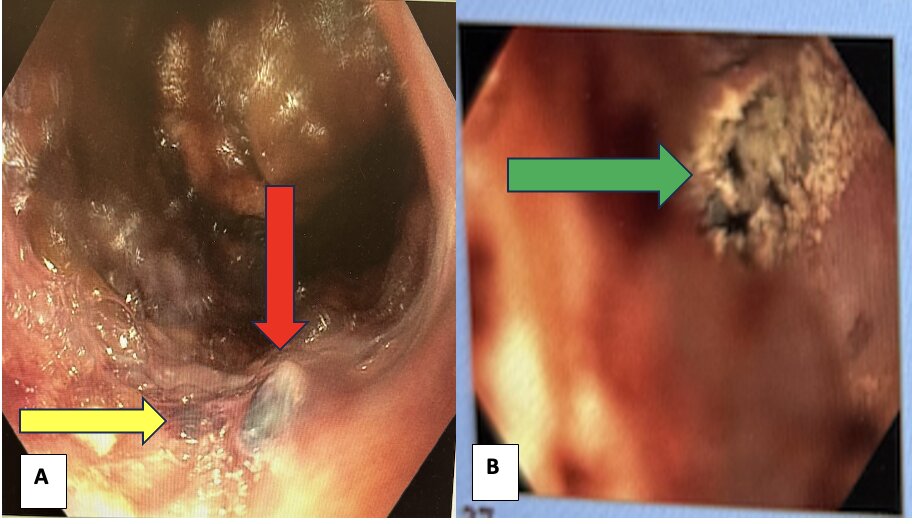
Figure: Figure1 A: Yellow arrow points to the base of the Dieulafoy's lesion with the Red Arrow pointing to the visible vessel identified in the lesion. Figure 1 B: Green Arrow points to the lesion post-treatment with epinephrine injection and hemospray.
Disclosures:
Annie Shergill indicated no relevant financial relationships.
Hayden Aaron indicated no relevant financial relationships.
Annie Shergill, MD1, Hayden Aaron, MD2. P2308 - Now You See It, Now You Don't - A Rare Cause of Non-Variceal Upper GI Bleeding in a Cirrhotic Patient: Esophageal Dieulafoy's Lesion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
