Monday Poster Session
Category: Esophagus
P2230 - Evaluating Risk Factors for Lymph Node Metastasis in Surgically Resected T1b Esophageal Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Omar Saab, MD
Cleveland Clinic Foundation
Westlake, OH
Presenting Author(s)
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4
1Cleveland Clinic Foundation, Westlake, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Endoscopic resection of low risk T1a cancer with ablation of remaining Barrett’s esophagus has become the standard of care for early Barrett’s neoplasia. T1b EAC are believed to have a higher risk of lymph node metastasis, and surgical resection is recommended. Many patients with T1b EAC are not surgical candidates, due to co-morbidities or patient preference, and are referred for endoscopic submucosal dissection (ESD). The esophageal submucosa is a watershed area, with risk of lymph node metastases rates ranging from 7 to 45%, but little evidence exists for risk factors for lymph node metastases in T1b EAC. Our study aims to investigate the risk factors associated with lymph node metastasis on surgically resected T1b EAC.
Methods: We performed a retrospective single center cohort study on 120 patients who had esophagectomy of pathologically staged T1b EAC, who had not received preoperative chemotherapy or radiation. Consecutive patients who underwent esophagectomy between 1988 and 2009 with pathology revealing T1b EAC were included. Pathologic specimens were re-revaluated by an expert GI pathologist for this study, and the exact depth of submucosal invasion was measured in microns. Tumors were histologically examined for micron-depth invasion, percentage of submucosal involvement, differentiation status, lymphovascular invasion (LVI), tumor location, tumor budding, and number of poorly differentiated clusters.
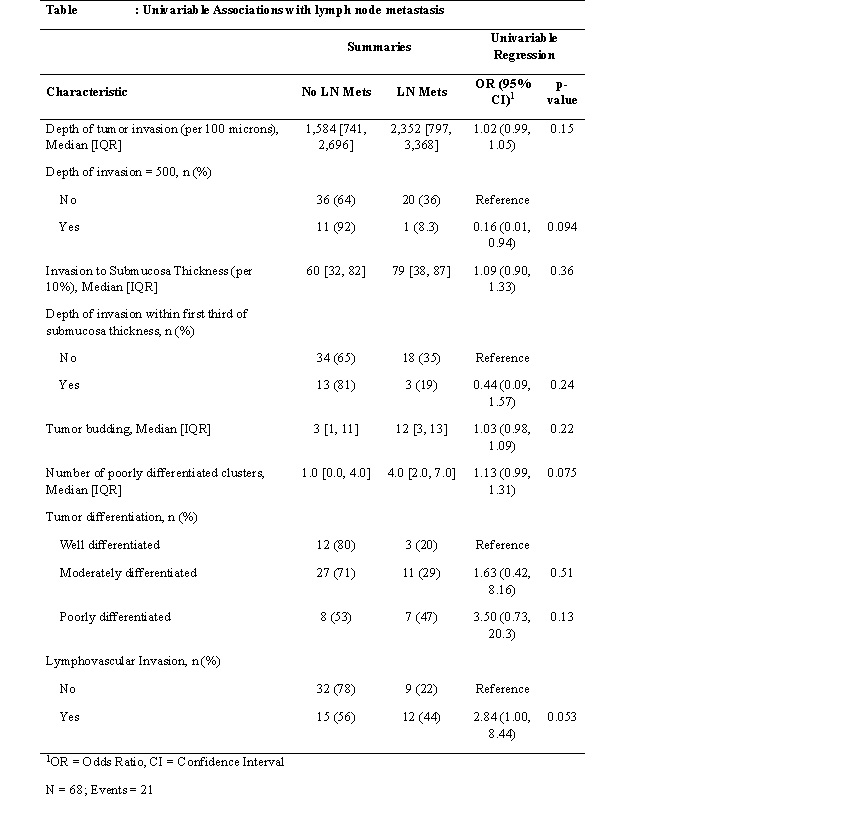
Results: Of 120 patients who under esophagectomy alone for T1b EAC, 68 with available pathologic samples were included in the analysis. The patient demographics and surgical details are presented on Table 1. The majority of patients had a thoracotomy approach (n=42, 62%), the median number of lymph nodes removed was 17 (11,27), and all patients had R0 resection. 21/69 (31%) had at least 1 positive lymph node at the time of surgery. Table 2 shows the univariable analysis of factors associated with lymph node metastasis.
Discussion: In T1b EAC, who are clinically staged as N0, positive lymph nodes were found 30% of the time at surgical resection. While there was a trend towards depth of submucosal invasion, lymphovascular invasion and grade of tumor being associated with lymph node metastasis this did not reach statistical significance. A larger sample size analysis may be required. In patients with clinically staged T1b N0, a high degree of suspicion is needed, as 30% in our study had positive lymph nodes at the time of surgery.
Disclosures:
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4. P2230 - Evaluating Risk Factors for Lymph Node Metastasis in Surgically Resected T1b Esophageal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Westlake, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Endoscopic resection of low risk T1a cancer with ablation of remaining Barrett’s esophagus has become the standard of care for early Barrett’s neoplasia. T1b EAC are believed to have a higher risk of lymph node metastasis, and surgical resection is recommended. Many patients with T1b EAC are not surgical candidates, due to co-morbidities or patient preference, and are referred for endoscopic submucosal dissection (ESD). The esophageal submucosa is a watershed area, with risk of lymph node metastases rates ranging from 7 to 45%, but little evidence exists for risk factors for lymph node metastases in T1b EAC. Our study aims to investigate the risk factors associated with lymph node metastasis on surgically resected T1b EAC.
Methods: We performed a retrospective single center cohort study on 120 patients who had esophagectomy of pathologically staged T1b EAC, who had not received preoperative chemotherapy or radiation. Consecutive patients who underwent esophagectomy between 1988 and 2009 with pathology revealing T1b EAC were included. Pathologic specimens were re-revaluated by an expert GI pathologist for this study, and the exact depth of submucosal invasion was measured in microns. Tumors were histologically examined for micron-depth invasion, percentage of submucosal involvement, differentiation status, lymphovascular invasion (LVI), tumor location, tumor budding, and number of poorly differentiated clusters.
Results: Of 120 patients who under esophagectomy alone for T1b EAC, 68 with available pathologic samples were included in the analysis. The patient demographics and surgical details are presented on Table 1. The majority of patients had a thoracotomy approach (n=42, 62%), the median number of lymph nodes removed was 17 (11,27), and all patients had R0 resection. 21/69 (31%) had at least 1 positive lymph node at the time of surgery. Table 2 shows the univariable analysis of factors associated with lymph node metastasis.
Discussion: In T1b EAC, who are clinically staged as N0, positive lymph nodes were found 30% of the time at surgical resection. While there was a trend towards depth of submucosal invasion, lymphovascular invasion and grade of tumor being associated with lymph node metastasis this did not reach statistical significance. A larger sample size analysis may be required. In patients with clinically staged T1b N0, a high degree of suspicion is needed, as 30% in our study had positive lymph nodes at the time of surgery.
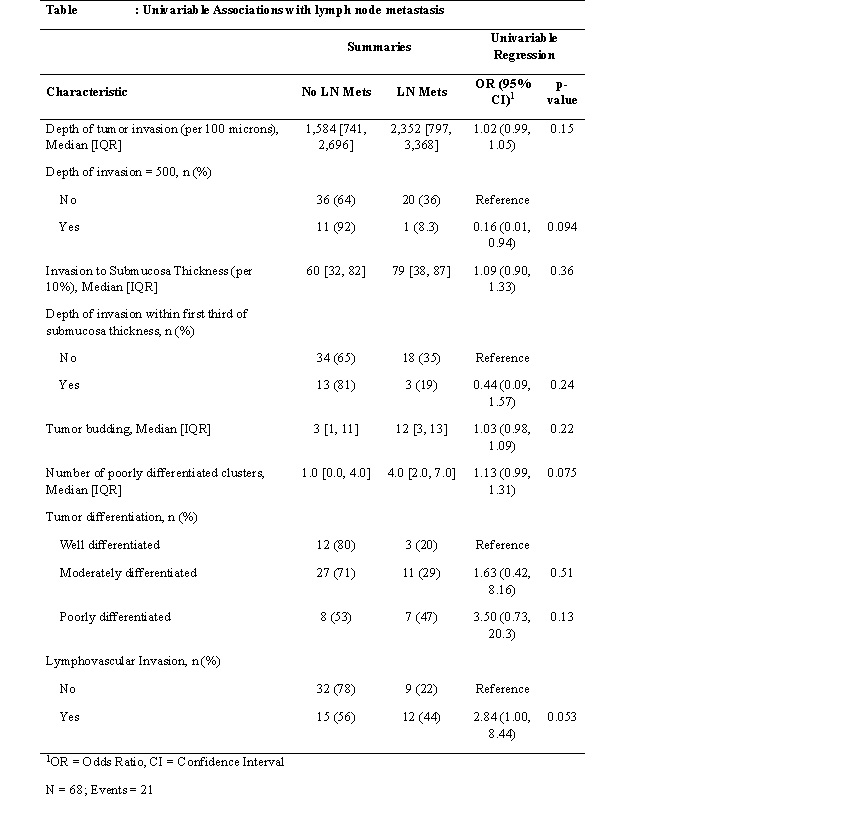
Figure: Risk factors
Disclosures:
Omar Saab indicated no relevant financial relationships.
Xuefeng Zhang indicated no relevant financial relationships.
James Bena indicated no relevant financial relationships.
Siva Raja indicated no relevant financial relationships.
Amit Bhatt indicated no relevant financial relationships.
Omar Saab, MD1, Xuefeng Zhang, MD2, James Bena, BS2, Siva Raja, MD3, Amit Bhatt, MD4. P2230 - Evaluating Risk Factors for Lymph Node Metastasis in Surgically Resected T1b Esophageal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
