Monday Poster Session
Category: Esophagus
P2242 - A Rare Case of an Atrioesophageal Fistula after a Maze Procedure
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Danzhu Zhao, DO
University of Connecticut Health Center
WEST HARTFORD, CT
Presenting Author(s)
Danzhu Zhao, DO1, Neil Khoury, MD2, Jose Pichardo-Castillo, MD3
1University of Connecticut Health Center, Farmington, CT; 2UConn Health, Hartford, CT; 3Hartford Hospital, Hartford, CT
Introduction: Atrioesophageal fistula (AEF) formation is a very rare but dangerous complication of atrial fibrillation (AF) ablation procedures. Patients may present with fevers, neurologic deficits and/or hematemesis (1). We present a case of a patient who presented with neurologic deficits 4 weeks after receiving a Maze procedure due to an AEF.
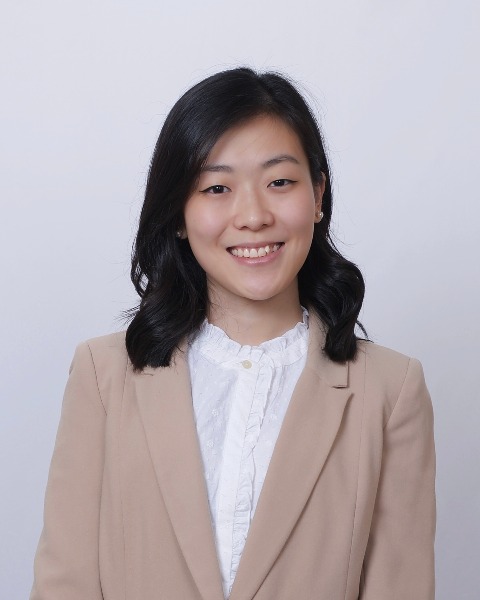
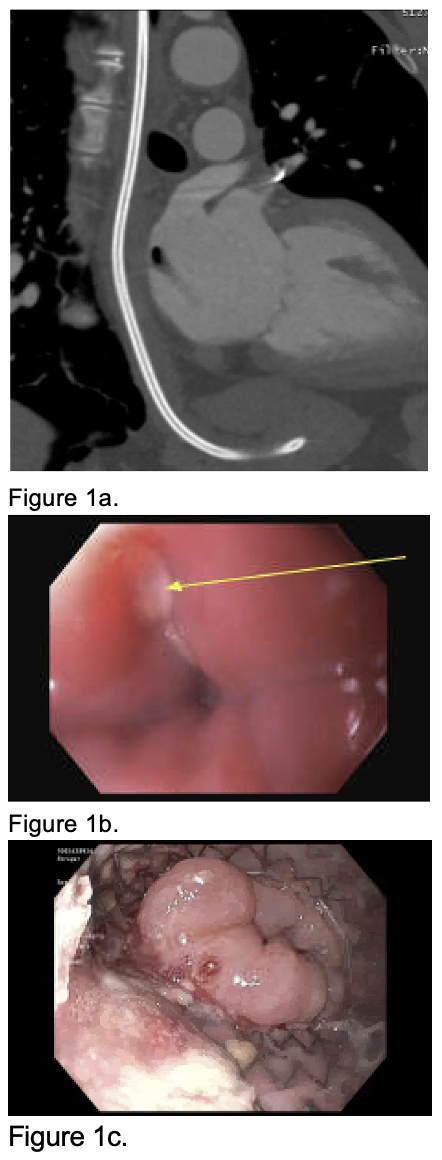
Case Description/Methods: A 59-year-old male with history of AF status post Maze procedure (4 weeks prior) presented to the hospital after a fall. He was afebrile, normotensive and non-tachycardic. On exam, his left upper extremity was contracted and he had decreased left lower extremity strength. Head CT revealed a cerebral air embolism along the right cerebrum. Thoracic CT imaging revealed an 8mm by 12 mm left atrial air emboli (Figure 1a). Blood work revealed leukocytosis (WBC 21.7K/uL). Broad spectrum antibiotics and antifungal therapy were initiated and he was taken to the operating room for left atrial fistula closure with a bovine pericardial patch. An upper endoscopy (EGD) confirmed a small fistulous opening 30cm from the incisors (Figure 1b) and a 23mm by 100mm fully covered esophageal metal stent was placed.
Subsequently, he developed dysphagia and anorexia. Repeat upper EGD revealed a partially obstructed stent from tissue overgrowth (Figure 1c). An overlapping telescoping stent was placed. Eventually, the fistula healed and the stent was removed. He was discharged to inpatient rehabilitation tolerating liquid diet by mouth and tube feeds through a gastric tube.
The patient was readmitted with septic shock from polymicrobial bacteremia due to recurrence of his AEF, confirmed on upper EGD. A 10mm fistula in the mid esophagus was closed with an over-the-scope clip. Subsequently, he went for definitive surgical repair with thoracic surgery.
Discussion: Although rare, serious complications such as AEF may occur 2-6 weeks after a Maze procedure. Gastroenterologists may be consulted for hematemesis in a patient with AEF. These patients will often have accompanying neurologic deficits. It is important to avoid endoscopy as air insufflation may exacerbate air emboli formation. Esophageal stenting or over-the-scope clips may be used as a bridge to surgical repair which has been shown to reduce mortality (1). There may be a role for prophylactic acid suppression in those undergoing AF ablation as peptic injury may predispose one to AEF formation.
References:
1. Han HC et al. Atrioesophageal Fistula. Circ Arrhythm Electrophysiol. 2017 Nov;10(11):e005579.
Disclosures:
Danzhu Zhao, DO1, Neil Khoury, MD2, Jose Pichardo-Castillo, MD3. P2242 - A Rare Case of an Atrioesophageal Fistula after a Maze Procedure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2UConn Health, Hartford, CT; 3Hartford Hospital, Hartford, CT
Introduction: Atrioesophageal fistula (AEF) formation is a very rare but dangerous complication of atrial fibrillation (AF) ablation procedures. Patients may present with fevers, neurologic deficits and/or hematemesis (1). We present a case of a patient who presented with neurologic deficits 4 weeks after receiving a Maze procedure due to an AEF.
Case Description/Methods: A 59-year-old male with history of AF status post Maze procedure (4 weeks prior) presented to the hospital after a fall. He was afebrile, normotensive and non-tachycardic. On exam, his left upper extremity was contracted and he had decreased left lower extremity strength. Head CT revealed a cerebral air embolism along the right cerebrum. Thoracic CT imaging revealed an 8mm by 12 mm left atrial air emboli (Figure 1a). Blood work revealed leukocytosis (WBC 21.7K/uL). Broad spectrum antibiotics and antifungal therapy were initiated and he was taken to the operating room for left atrial fistula closure with a bovine pericardial patch. An upper endoscopy (EGD) confirmed a small fistulous opening 30cm from the incisors (Figure 1b) and a 23mm by 100mm fully covered esophageal metal stent was placed.
Subsequently, he developed dysphagia and anorexia. Repeat upper EGD revealed a partially obstructed stent from tissue overgrowth (Figure 1c). An overlapping telescoping stent was placed. Eventually, the fistula healed and the stent was removed. He was discharged to inpatient rehabilitation tolerating liquid diet by mouth and tube feeds through a gastric tube.
The patient was readmitted with septic shock from polymicrobial bacteremia due to recurrence of his AEF, confirmed on upper EGD. A 10mm fistula in the mid esophagus was closed with an over-the-scope clip. Subsequently, he went for definitive surgical repair with thoracic surgery.
Discussion: Although rare, serious complications such as AEF may occur 2-6 weeks after a Maze procedure. Gastroenterologists may be consulted for hematemesis in a patient with AEF. These patients will often have accompanying neurologic deficits. It is important to avoid endoscopy as air insufflation may exacerbate air emboli formation. Esophageal stenting or over-the-scope clips may be used as a bridge to surgical repair which has been shown to reduce mortality (1). There may be a role for prophylactic acid suppression in those undergoing AF ablation as peptic injury may predispose one to AEF formation.
References:
1. Han HC et al. Atrioesophageal Fistula. Circ Arrhythm Electrophysiol. 2017 Nov;10(11):e005579.
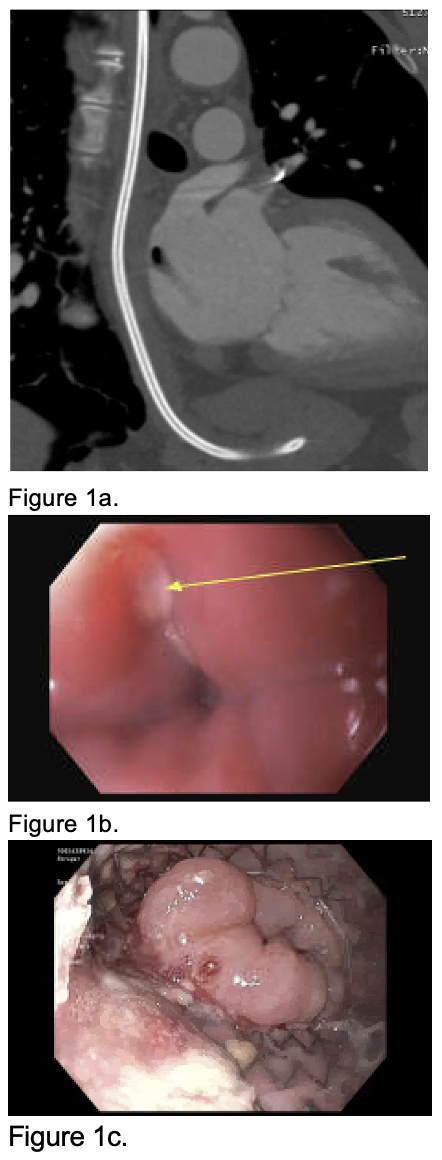
Figure: Figure 1a. Thoracic CT image revealing an irregularly-shaped 8mm x 12 mm low-attenuation focus in the left atrium concerning for an air embolus.
Figure 1b.There was a small fistulous opening noted at 30 cm from incisors confirmed on upper endoscopy.
Figure 1c. An esophageal stent was found in the middle third of the esophagus with a partially obstructive tissue overgrowth at the distal aspect of the stent on repeat endoscopy.
Figure 1b.There was a small fistulous opening noted at 30 cm from incisors confirmed on upper endoscopy.
Figure 1c. An esophageal stent was found in the middle third of the esophagus with a partially obstructive tissue overgrowth at the distal aspect of the stent on repeat endoscopy.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Neil Khoury indicated no relevant financial relationships.
Jose Pichardo-Castillo indicated no relevant financial relationships.
Danzhu Zhao, DO1, Neil Khoury, MD2, Jose Pichardo-Castillo, MD3. P2242 - A Rare Case of an Atrioesophageal Fistula after a Maze Procedure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
