Monday Poster Session
Category: Colorectal Cancer Prevention
P2158 - Root Cause Analysis of Post-Colonoscopy Colorectal Cancer in FIT-Positive Individuals: Results From A Nationwide Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Natalie Wilson, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Natalie Wilson, MD1, Rahul Karna, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 5NYU Langone Health, New York, NY
Introduction: Post-colonoscopy colorectal cancer (PCCRC) is defined as CRC diagnosed six months or later after a colonoscopy in which no cancer is identified. The World Endoscopy Organization (WEO) has proposed guidelines for categorization of PCCRCs. The aim of this study is to apply the WEO categorization and perform a root cause analysis (RCA) of PCCRCs in fecal immunochemical (FIT)-positive individuals using a nationwide cohort.
Methods: Data was obtained from the Veterans Health Administration Corporate Data Warehouse. Individuals who underwent their first colonoscopy after a positive FIT between January 2015 and August 2023 were included. PCCRCs were identified using the VA Central Cancer Registry and Systematized Nomenclature of Medicine codes. PCCRC was defined per WEO guidelines as CRC diagnosed 6 to 48 months after colonoscopy where no CRC was identified.
All available records were reviewed for each potential PCCRC. PCCRCs were then categorized per the WEO system as interval (diagnosed before the recommended surveillance interval) or non-interval type A (diagnosed at the recommended surveillance interval), type B (diagnosed after recommended surveillance interval), or type C (diagnosed when no surveillance interval was recommended). The appropriateness of recommended surveillance intervals based on guideline recommendations was also evaluated. An RCA was then performed to determine the most plausible etiology of PCCRC.
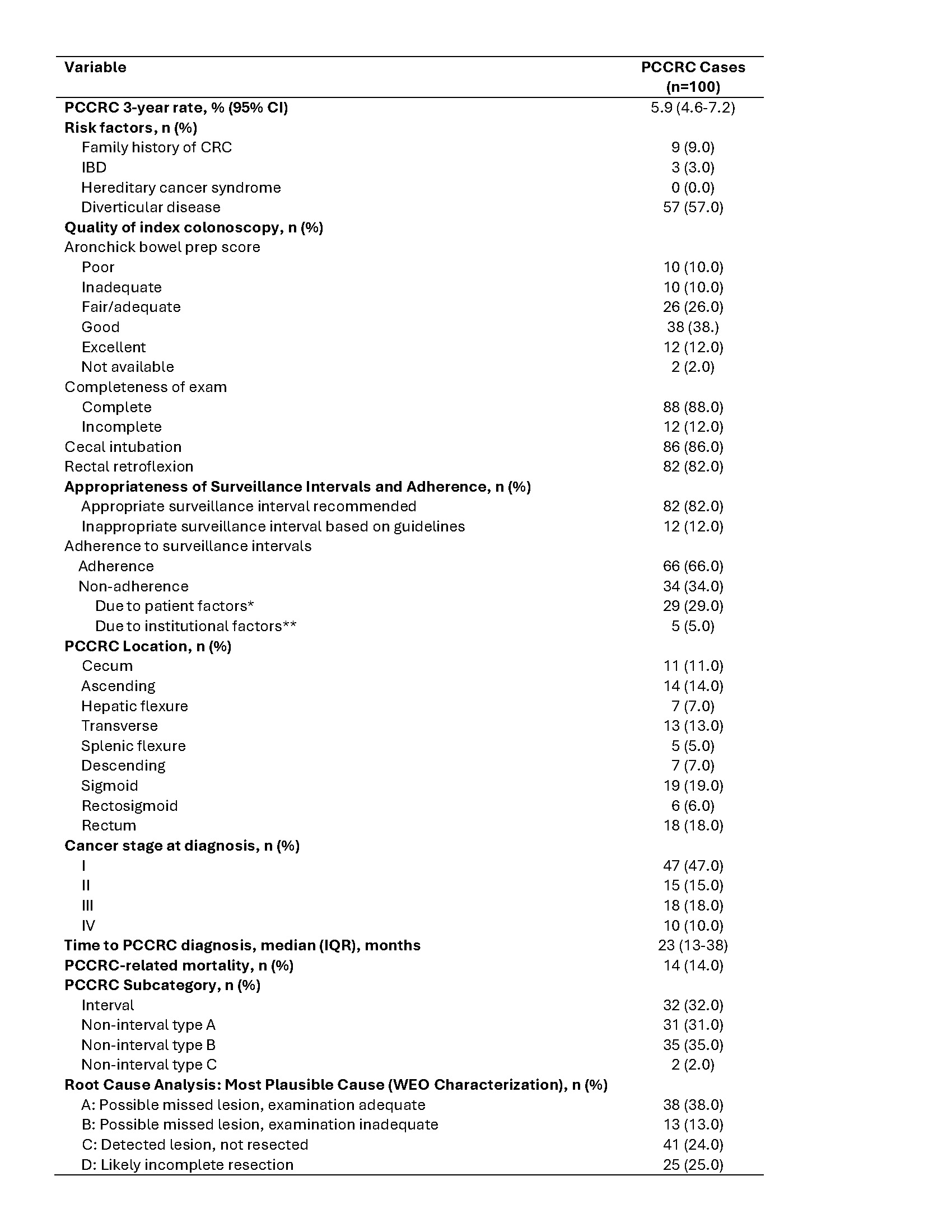
Results: A total of 52,167 colonoscopies were performed after a positive FIT [Table 1]. 100 cases of PCCRC were identified.
The median time to PCCRC diagnosis was 23 months. 75 PCCRCs were diagnosed within 3 years, resulting in a PCCRC 3-year rate of 5.9% (95% CI: 4.6%–7.2%). Subcategories of PCCRCs were as follows: interval (32%), non-interval type A (31%), type B (35%), type C (2%). Inappropriate surveillance interval was recommended in 12% of cases and accounted for 11 interval PCCRCs. The most common plausible etiology for PCCRC was possible missed lesion with adequate exam (38%) followed by incompletely resected lesion (25%), detected lesion that was not resected (24%), and missed lesion with inadequate exam (13%). PCCRC-related mortality rate was 14% [Table 2].
Discussion: Missed lesions and incomplete lesion resection were the most common plausible causes of PCCRC. This reinforces the importance of second look in the proximal colon and development of quality metrics focusing on polypectomy technique.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Natalie Wilson, MD1, Rahul Karna, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5. P2158 - Root Cause Analysis of Post-Colonoscopy Colorectal Cancer in FIT-Positive Individuals: Results From A Nationwide Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 5NYU Langone Health, New York, NY
Introduction: Post-colonoscopy colorectal cancer (PCCRC) is defined as CRC diagnosed six months or later after a colonoscopy in which no cancer is identified. The World Endoscopy Organization (WEO) has proposed guidelines for categorization of PCCRCs. The aim of this study is to apply the WEO categorization and perform a root cause analysis (RCA) of PCCRCs in fecal immunochemical (FIT)-positive individuals using a nationwide cohort.
Methods: Data was obtained from the Veterans Health Administration Corporate Data Warehouse. Individuals who underwent their first colonoscopy after a positive FIT between January 2015 and August 2023 were included. PCCRCs were identified using the VA Central Cancer Registry and Systematized Nomenclature of Medicine codes. PCCRC was defined per WEO guidelines as CRC diagnosed 6 to 48 months after colonoscopy where no CRC was identified.
All available records were reviewed for each potential PCCRC. PCCRCs were then categorized per the WEO system as interval (diagnosed before the recommended surveillance interval) or non-interval type A (diagnosed at the recommended surveillance interval), type B (diagnosed after recommended surveillance interval), or type C (diagnosed when no surveillance interval was recommended). The appropriateness of recommended surveillance intervals based on guideline recommendations was also evaluated. An RCA was then performed to determine the most plausible etiology of PCCRC.
Results: A total of 52,167 colonoscopies were performed after a positive FIT [Table 1]. 100 cases of PCCRC were identified.
The median time to PCCRC diagnosis was 23 months. 75 PCCRCs were diagnosed within 3 years, resulting in a PCCRC 3-year rate of 5.9% (95% CI: 4.6%–7.2%). Subcategories of PCCRCs were as follows: interval (32%), non-interval type A (31%), type B (35%), type C (2%). Inappropriate surveillance interval was recommended in 12% of cases and accounted for 11 interval PCCRCs. The most common plausible etiology for PCCRC was possible missed lesion with adequate exam (38%) followed by incompletely resected lesion (25%), detected lesion that was not resected (24%), and missed lesion with inadequate exam (13%). PCCRC-related mortality rate was 14% [Table 2].
Discussion: Missed lesions and incomplete lesion resection were the most common plausible causes of PCCRC. This reinforces the importance of second look in the proximal colon and development of quality metrics focusing on polypectomy technique.
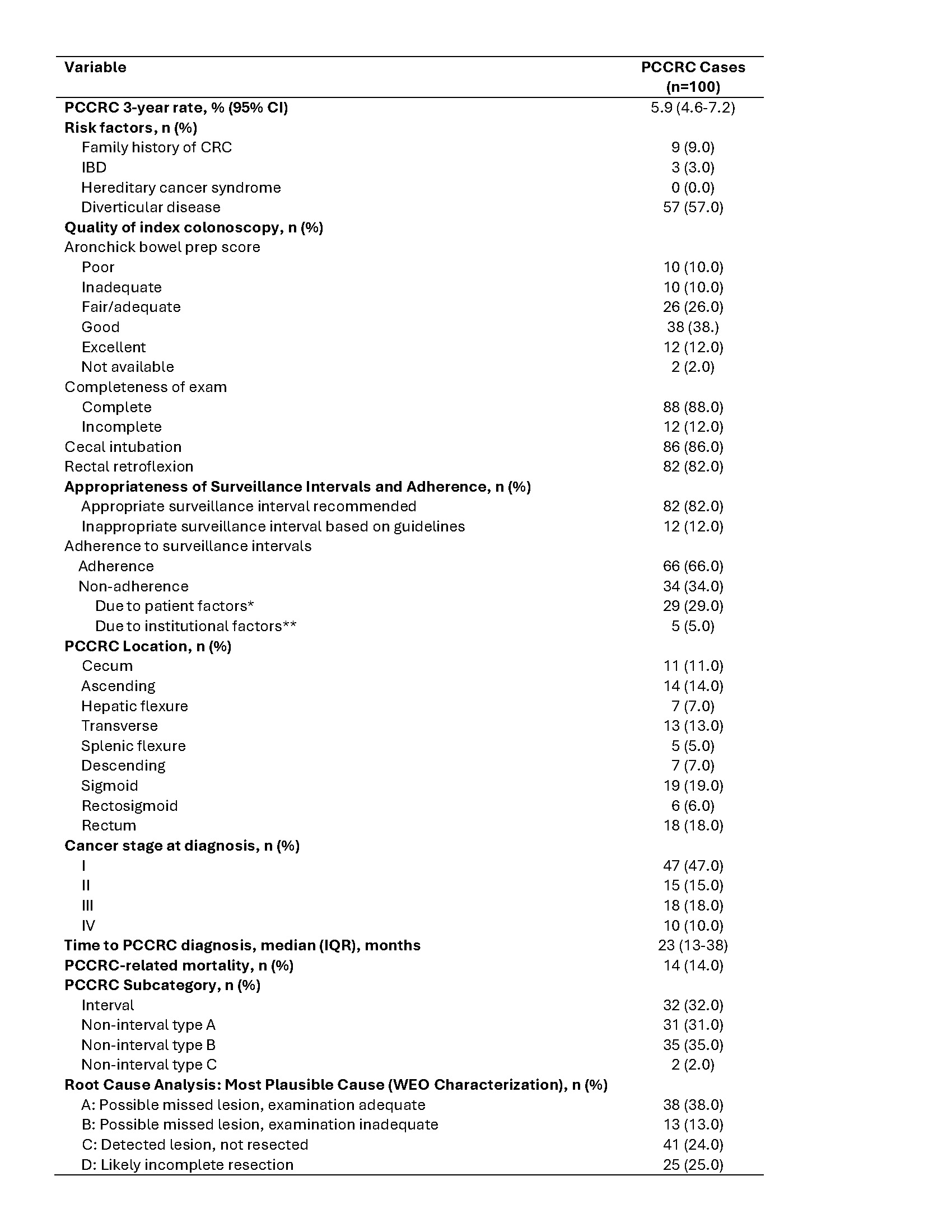
Figure: Table 2. Characteristics of PCCRC and Root Cause Analysis
Abbreviations: PCCRC: post-colonoscopy colorectal cancer; IBD: inflammatory bowel disease; IQR: interquartile range
*Patent factors include comorbidities that may delay surveillance endoscopy or patient choice or patient is lost to follow-up
**Administrative factors include scheduling delays or postponed procedures due to institutional factors such as during COVID-19 pandemic
Abbreviations: PCCRC: post-colonoscopy colorectal cancer; IBD: inflammatory bowel disease; IQR: interquartile range
*Patent factors include comorbidities that may delay surveillance endoscopy or patient choice or patient is lost to follow-up
**Administrative factors include scheduling delays or postponed procedures due to institutional factors such as during COVID-19 pandemic
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Anders Westanmo indicated no relevant financial relationships.
Amy Gravely indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Aasma Shaukat: iterative health; Freenome – Consultant.
Natalie Wilson, MD1, Rahul Karna, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Mohammad Bilal, MD4, Aasma Shaukat, MD, MPH5. P2158 - Root Cause Analysis of Post-Colonoscopy Colorectal Cancer in FIT-Positive Individuals: Results From A Nationwide Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
