Monday Poster Session
Category: Colon
P2062 - Primary Campylobacter Colitis Masquerading as Clostridium difficile Pseudomembranous Colitis: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hind El Naamani, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Hind El Naamani, MD
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Pseudomembranous colitis (PMC) is commonly linked to Clostridium difficile infection (CDI) but can also be caused by other infectious and non-infectious factors. This case report highlights a rare instance of PMC caused by Campylobacter jejuni in a patient with abdominal pain and bloody stool. To our knowledge, this is the first reported case of Campylobacter-induced PMC.
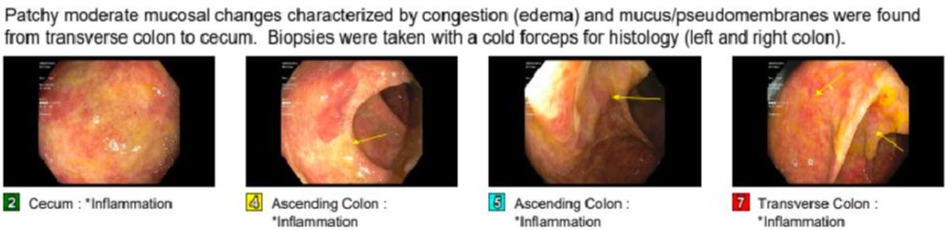
Case Description/Methods: A 67-year-old female with a history of colonic polyps and hyperparathyroidism presented with persistent abdominal pain and bloody stools/mucus lasting over a month. Lab results showed normal white blood cell count, Erythrocyte Sedimentation Rate 6 mm/h, C-reactive protein 1.1 mg/l and fecal calprotectin 52 mcg/g. Stool studies were negative for ova or parasites, salmonella, shigella, campylobacter and Clostridium difficile (Glutamate Dehydrogenase negative and toxin A/B negative).Colonoscopy revealed patchy moderate mucosal changes resembling pseudomembranes from the transverse colon to the cecum, with a normal terminal ileum.Biopsy revealed active colitis especially in the right colon. Colonic mucosa showed cryptitis, crypt abscess and no granuloma. A later culture from the colonoscopy tested positive for Campylobacter. The patient's symptoms resolved naturally without treatment. Follow-up CT enterography two months later showed no signs of acute focal inflammation in the bowel and a normal ileum.
Discussion: Campylobacter is a leading cause of diarrhea globally, with approximately 1.3 million cases annually in the U.S. It spreads through contaminated food, water, animal contact, and person-to-person transmission. Diagnosis is made through stool tests, and treatment is typically supportive, with antibiotics reserved for severe cases.PMC is commonly associated with CDI but can also result from various other infectious and non-infectious agents. In this case, a patient with no typical PMC risk factors and a distant history of colitis initially tested negative for infectious causes and was suspected of having late-onset inflammatory bowel disease (IBD). However, a subsequent colonoscopy biopsy revealed Campylobacter infection. Her symptoms resolved without intervention, and follow-up imaging confirmed the resolution of inflammatory changes. This unique presentation highlights the need to consider a broad range of causes for PMC beyond CDI. Although no previous cases of campylobacter-induced PMC have been reported, there are documented instances of Campylobacter presenting with features similar to IBD.
Disclosures:
Hind El Naamani, MD. P2062 - Primary <i>Campylobacter</i> Colitis Masquerading as <i>Clostridium difficile</i> Pseudomembranous Colitis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Pseudomembranous colitis (PMC) is commonly linked to Clostridium difficile infection (CDI) but can also be caused by other infectious and non-infectious factors. This case report highlights a rare instance of PMC caused by Campylobacter jejuni in a patient with abdominal pain and bloody stool. To our knowledge, this is the first reported case of Campylobacter-induced PMC.
Case Description/Methods: A 67-year-old female with a history of colonic polyps and hyperparathyroidism presented with persistent abdominal pain and bloody stools/mucus lasting over a month. Lab results showed normal white blood cell count, Erythrocyte Sedimentation Rate 6 mm/h, C-reactive protein 1.1 mg/l and fecal calprotectin 52 mcg/g. Stool studies were negative for ova or parasites, salmonella, shigella, campylobacter and Clostridium difficile (Glutamate Dehydrogenase negative and toxin A/B negative).Colonoscopy revealed patchy moderate mucosal changes resembling pseudomembranes from the transverse colon to the cecum, with a normal terminal ileum.Biopsy revealed active colitis especially in the right colon. Colonic mucosa showed cryptitis, crypt abscess and no granuloma. A later culture from the colonoscopy tested positive for Campylobacter. The patient's symptoms resolved naturally without treatment. Follow-up CT enterography two months later showed no signs of acute focal inflammation in the bowel and a normal ileum.
Discussion: Campylobacter is a leading cause of diarrhea globally, with approximately 1.3 million cases annually in the U.S. It spreads through contaminated food, water, animal contact, and person-to-person transmission. Diagnosis is made through stool tests, and treatment is typically supportive, with antibiotics reserved for severe cases.PMC is commonly associated with CDI but can also result from various other infectious and non-infectious agents. In this case, a patient with no typical PMC risk factors and a distant history of colitis initially tested negative for infectious causes and was suspected of having late-onset inflammatory bowel disease (IBD). However, a subsequent colonoscopy biopsy revealed Campylobacter infection. Her symptoms resolved without intervention, and follow-up imaging confirmed the resolution of inflammatory changes. This unique presentation highlights the need to consider a broad range of causes for PMC beyond CDI. Although no previous cases of campylobacter-induced PMC have been reported, there are documented instances of Campylobacter presenting with features similar to IBD.
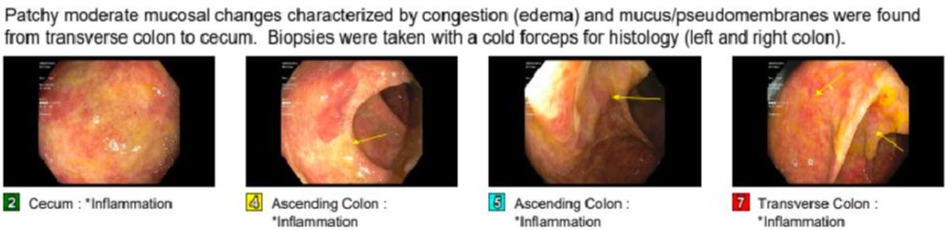
Figure: Colonoscopy Images
Disclosures:
Hind El Naamani indicated no relevant financial relationships.
Hind El Naamani, MD. P2062 - Primary <i>Campylobacter</i> Colitis Masquerading as <i>Clostridium difficile</i> Pseudomembranous Colitis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
