Monday Poster Session
Category: Colon
P2068 - The Art of Disguise: CMV Masquerading as Colonic Malignancy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Pranay Reddy, MD, MPH
University of Kansas Medical Center
Kansas City, KS
Presenting Author(s)
Pranay Reddy, MD, MPH, Sohini Samaddar, MBBS, James Langworthy, MD
University of Kansas Medical Center, Kansas City, KS
Introduction: Cytomegalovirus (CMV) is a double-stranded DNA virus belonging to the Herpesviridae family. It is ubiquitous and infects the majority of humans at some point in their lives, with serology indicating prior exposure in 40-100% of individuals. In immunocompetent patients, CMV usually presents as a viral syndrome or mononucleosis-like illness. In immunocompromised patients however, the manifestations can be more severe with colitis being the predominant extraocular presentation. Rare presentations include toxic megacolon, perforation, appendicitis and pseudotumors. We discuss one such case of a patient with tissue invasive gastrointestinal CMV infection masquerading as colonic malignancy.
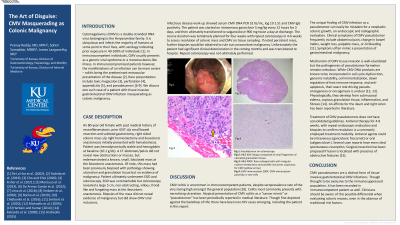
Case Description/Methods: An 80-year old female with past medical history of neurofibromatosis, prior GIST s/p small bowel resection and subtotal gastrectomy, right sided colonic mass s/p right hemicolectomy and ileocolonic anastomosis initially presented with hematochezia. Patient was hemodynamically stable and hemoglobin at baseline (10.1 g/dL). A CT abdomen/pelvis did not reveal new obstructions or masses, but redemonstrated a known, small, lobulated mass at the ileocolonic anastomosis. Of note, this mass had been previously biopsied with pathology showing ulceration and granulation tissue but no evidence of malignancy. Patient ultimately underwent EGD and colonoscopy. EGD was unremarkable but colonoscopy revealed a large 5 cm, non-obstructing, villous, frond-like and fungating mass at the ileocolonic anastomosis. Biopsies of the mass did not reveal evidence of malignancy but did show CMV viral inclusions. Infectious disease work up showed serum CMV DNA PCR 32 IU/mL, log 10 1.51 and CMV IgG positivity. The patient was started on intravenous ganciclovir 5 mg/kg every 12 hours for 3 days, and then ultimately transitioned to valganciclovir 900 mg twice a day at discharge. The course duration was tentatively planned for four weeks with repeat colonoscopy in 4-6 weeks to assess resolution of colonic mass. If noted persistent mass, further biopsies would be obtained to rule out concomitant malignancy.
Discussion: CMV pseudotumors are a distinctive form of tissue-invasive gastrointestinal CMV infections. Though thought to be exclusive to the immunosuppressed population, it has been recorded in immunocompetent patients as well. Clinicians should be aware of this possible differential when evaluating colonic masses, even in the absence of traditional risk factors.

Disclosures:
Pranay Reddy, MD, MPH, Sohini Samaddar, MBBS, James Langworthy, MD. P2068 - The Art of Disguise: CMV Masquerading as Colonic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Kansas Medical Center, Kansas City, KS
Introduction: Cytomegalovirus (CMV) is a double-stranded DNA virus belonging to the Herpesviridae family. It is ubiquitous and infects the majority of humans at some point in their lives, with serology indicating prior exposure in 40-100% of individuals. In immunocompetent patients, CMV usually presents as a viral syndrome or mononucleosis-like illness. In immunocompromised patients however, the manifestations can be more severe with colitis being the predominant extraocular presentation. Rare presentations include toxic megacolon, perforation, appendicitis and pseudotumors. We discuss one such case of a patient with tissue invasive gastrointestinal CMV infection masquerading as colonic malignancy.
Case Description/Methods: An 80-year old female with past medical history of neurofibromatosis, prior GIST s/p small bowel resection and subtotal gastrectomy, right sided colonic mass s/p right hemicolectomy and ileocolonic anastomosis initially presented with hematochezia. Patient was hemodynamically stable and hemoglobin at baseline (10.1 g/dL). A CT abdomen/pelvis did not reveal new obstructions or masses, but redemonstrated a known, small, lobulated mass at the ileocolonic anastomosis. Of note, this mass had been previously biopsied with pathology showing ulceration and granulation tissue but no evidence of malignancy. Patient ultimately underwent EGD and colonoscopy. EGD was unremarkable but colonoscopy revealed a large 5 cm, non-obstructing, villous, frond-like and fungating mass at the ileocolonic anastomosis. Biopsies of the mass did not reveal evidence of malignancy but did show CMV viral inclusions. Infectious disease work up showed serum CMV DNA PCR 32 IU/mL, log 10 1.51 and CMV IgG positivity. The patient was started on intravenous ganciclovir 5 mg/kg every 12 hours for 3 days, and then ultimately transitioned to valganciclovir 900 mg twice a day at discharge. The course duration was tentatively planned for four weeks with repeat colonoscopy in 4-6 weeks to assess resolution of colonic mass. If noted persistent mass, further biopsies would be obtained to rule out concomitant malignancy.
Discussion: CMV pseudotumors are a distinctive form of tissue-invasive gastrointestinal CMV infections. Though thought to be exclusive to the immunosuppressed population, it has been recorded in immunocompetent patients as well. Clinicians should be aware of this possible differential when evaluating colonic masses, even in the absence of traditional risk factors.

Figure: Colonic mass at ileocolonic anastomosis. Biopsies showing CMV.
Disclosures:
Pranay Reddy indicated no relevant financial relationships.
Sohini Samaddar indicated no relevant financial relationships.
James Langworthy indicated no relevant financial relationships.
Pranay Reddy, MD, MPH, Sohini Samaddar, MBBS, James Langworthy, MD. P2068 - The Art of Disguise: CMV Masquerading as Colonic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
