Monday Poster Session
Category: Colon
P2077 - Spotting the Culprit; HSP Vasculitis Presenting as a Massive Lower GI Hemorrhage in an Adult Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mitchelle V. Zolotarevsky, MD
University of Chicago, NorthShore Internal Medicine
Chicago, IL
Presenting Author(s)
Mitchelle V. Zolotarevsky, MD1, Kevin Khoury, MD2, Raza Muhammad, DO3, Maryam Haider, MD2, Michael Sprang, MD4, Edward Villa, MD4, David Labowitz, DO4
1University of Chicago, NorthShore Internal Medicine, Chicago, IL; 2University of Chicago Northshore, Evanston, IL; 3University of Chicago Endeavor Health, Evanston, IL; 4NorthShore University HealthSystem, Evanston, IL
Introduction: IgA Vasculitis, formerly Henoch-Schoenlein Purpura, involves immune complex deposition leading to skin purpura, arthralgias, renal impairment, and gastrointestinal involvement. The syndrome mainly presents in children but rarely can be seen in adults. Colicky pain from submucosal hemorrhage caused by vasculitis in the small bowel is common. A few cases of lower gastrointestinal bleeding are reported, but this is a rare finding. We present a unique case of an adult patient with classic findings of IgA vasculitis whose GI involvement led to hemorrhagic shock.
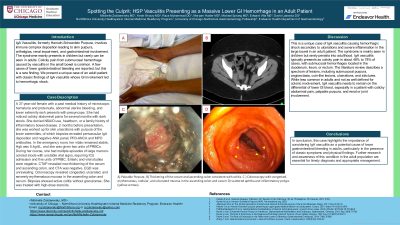
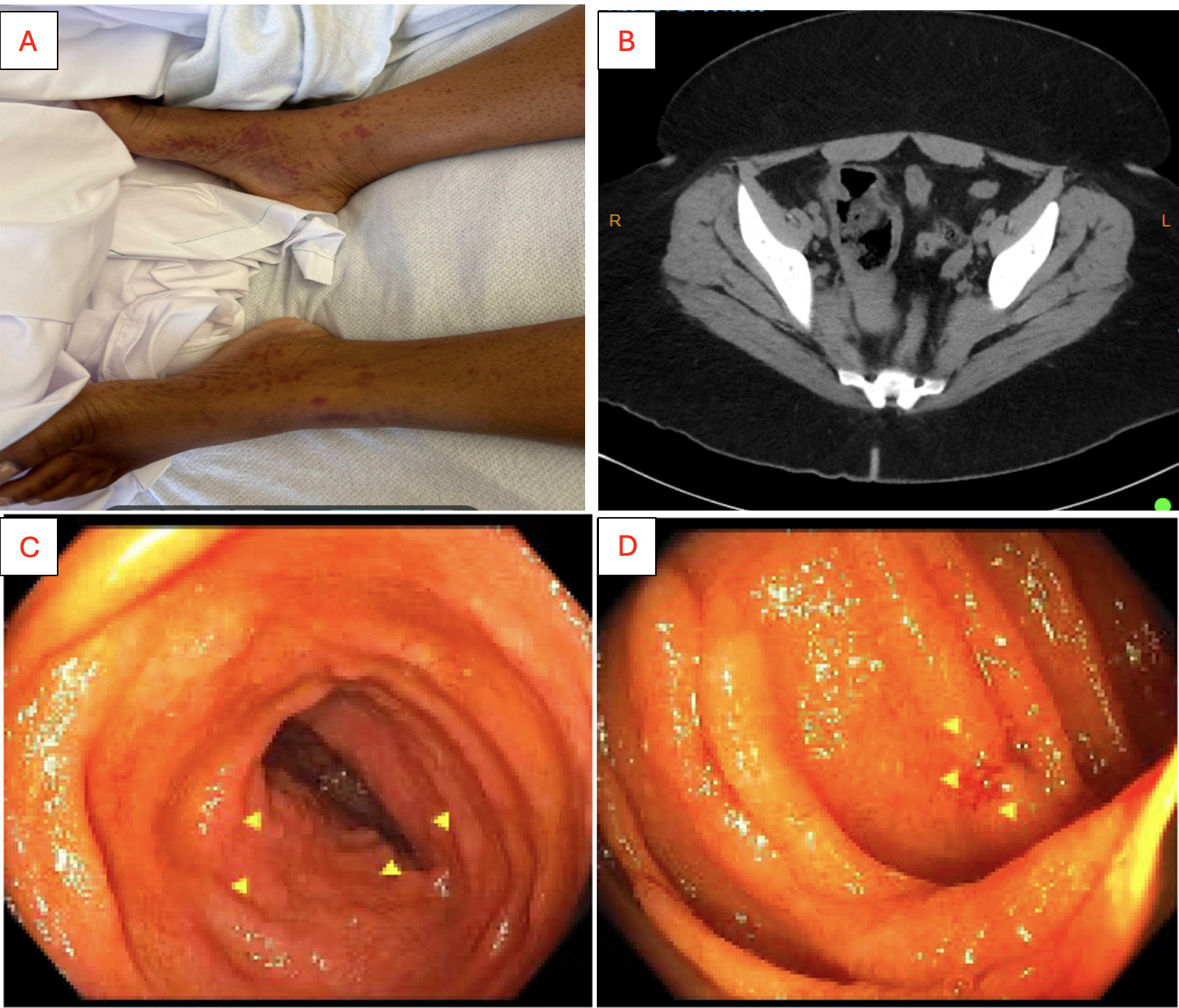
Case Description/Methods: A 37-year-old female with a past medical history of microscopic hematuria and proteinuria, abnormal uterine bleeding, and lower extremity rash presents with presyncope. She had noticed colicky abdominal pains for several months with dark stools. She denied NSAID use, heartburn, or a family history of inflammatory bowel disease. 2 months before presentation, she was worked up for skin ulcerations with purpura of the lower extremities, of which biopsies revealed perivascular IgA deposition and negative ANA panel, PR3-ANCA and MPO antibodies. In the emergency room, her vitals remained stable, Hgb was 5.4g/dL, and she was given two units of pRBCs. During her course, she had multiple episodes of large maroon-colored stools with unstable vital signs, requiring ICU admission and five units of pRBC. Enteric and viral studies were negative. CTAP revealed new thickening of the cecum and ascending colon, and CTA was negative. EGD was unrevealing. Colonoscopy revealed congested, ulcerated, and severely erythematous mucosa in the ascending colon and cecum. Biopsies showed active colitis without granulomas. She was treated with high-dose steroids.
Discussion: This is a unique case of IgA vasculitis causing hemorrhagic shock secondary to ulcerations and severe inflammation in the large bowel in an adult patient. The syndrome is mainly seen in children but rarely persists into adulthood. IgA vasculitis typically presents as colicky pain in about 48% to 78% of cases, with submucosal hemorrhages located in the duodenum, ileum, or rectum. The literature review describes a spectrum of lesions, including submucosal purpura, angioectasia, coin-like lesions, ulcerations, and strictures. While less common in adults and not as well defined for colonic involvement, IgA vasculitis needs to remain on the differential of lower GI bleed, especially in a patient with colicky abdominal pain, palpable purpura, and renal or joint involvement.
Disclosures:
Mitchelle V. Zolotarevsky, MD1, Kevin Khoury, MD2, Raza Muhammad, DO3, Maryam Haider, MD2, Michael Sprang, MD4, Edward Villa, MD4, David Labowitz, DO4. P2077 - Spotting the Culprit; HSP Vasculitis Presenting as a Massive Lower GI Hemorrhage in an Adult Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago, NorthShore Internal Medicine, Chicago, IL; 2University of Chicago Northshore, Evanston, IL; 3University of Chicago Endeavor Health, Evanston, IL; 4NorthShore University HealthSystem, Evanston, IL
Introduction: IgA Vasculitis, formerly Henoch-Schoenlein Purpura, involves immune complex deposition leading to skin purpura, arthralgias, renal impairment, and gastrointestinal involvement. The syndrome mainly presents in children but rarely can be seen in adults. Colicky pain from submucosal hemorrhage caused by vasculitis in the small bowel is common. A few cases of lower gastrointestinal bleeding are reported, but this is a rare finding. We present a unique case of an adult patient with classic findings of IgA vasculitis whose GI involvement led to hemorrhagic shock.
Case Description/Methods: A 37-year-old female with a past medical history of microscopic hematuria and proteinuria, abnormal uterine bleeding, and lower extremity rash presents with presyncope. She had noticed colicky abdominal pains for several months with dark stools. She denied NSAID use, heartburn, or a family history of inflammatory bowel disease. 2 months before presentation, she was worked up for skin ulcerations with purpura of the lower extremities, of which biopsies revealed perivascular IgA deposition and negative ANA panel, PR3-ANCA and MPO antibodies. In the emergency room, her vitals remained stable, Hgb was 5.4g/dL, and she was given two units of pRBCs. During her course, she had multiple episodes of large maroon-colored stools with unstable vital signs, requiring ICU admission and five units of pRBC. Enteric and viral studies were negative. CTAP revealed new thickening of the cecum and ascending colon, and CTA was negative. EGD was unrevealing. Colonoscopy revealed congested, ulcerated, and severely erythematous mucosa in the ascending colon and cecum. Biopsies showed active colitis without granulomas. She was treated with high-dose steroids.
Discussion: This is a unique case of IgA vasculitis causing hemorrhagic shock secondary to ulcerations and severe inflammation in the large bowel in an adult patient. The syndrome is mainly seen in children but rarely persists into adulthood. IgA vasculitis typically presents as colicky pain in about 48% to 78% of cases, with submucosal hemorrhages located in the duodenum, ileum, or rectum. The literature review describes a spectrum of lesions, including submucosal purpura, angioectasia, coin-like lesions, ulcerations, and strictures. While less common in adults and not as well defined for colonic involvement, IgA vasculitis needs to remain on the differential of lower GI bleed, especially in a patient with colicky abdominal pain, palpable purpura, and renal or joint involvement.
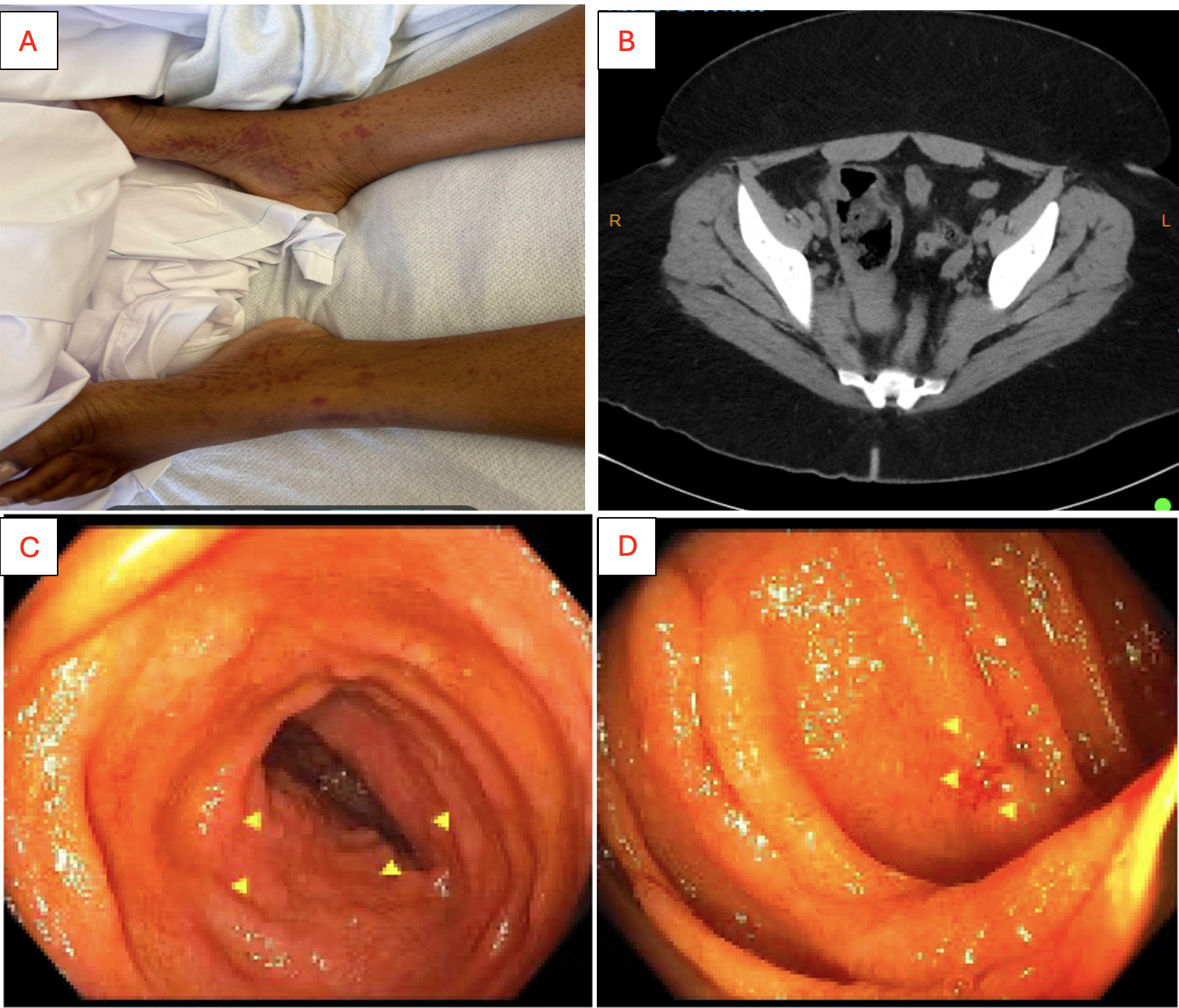
Figure: A) Palpable Purpura. B) Thickening of the cecum and ascending colon consistent with colitis. C and D) Colonoscopy with congested, erythematous, nodular, and ulcerated mucosa (yellow arrows) in the ascending colon and cecum with scattered aphtha and inflammatory polyps.
Disclosures:
Mitchelle Zolotarevsky indicated no relevant financial relationships.
Kevin Khoury indicated no relevant financial relationships.
Raza Muhammad indicated no relevant financial relationships.
Maryam Haider indicated no relevant financial relationships.
Michael Sprang indicated no relevant financial relationships.
Edward Villa: Interscope – Consultant. Olympus corp – Consultant.
David Labowitz indicated no relevant financial relationships.
Mitchelle V. Zolotarevsky, MD1, Kevin Khoury, MD2, Raza Muhammad, DO3, Maryam Haider, MD2, Michael Sprang, MD4, Edward Villa, MD4, David Labowitz, DO4. P2077 - Spotting the Culprit; HSP Vasculitis Presenting as a Massive Lower GI Hemorrhage in an Adult Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
