Monday Poster Session
Category: Colon
P2017 - The Great Mimicker: Intestinal Tuberculosis Masquerading as Colorectal Cancer
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RP
Rayna Patel, MD
University of Toledo College Medicine and Life Sciences
Grosse Pointe Woods, MI
Presenting Author(s)
Rayna Patel, MD1, Sahithi Chinnam, DO2, Sami Ghazaleh, MD3, Yaseen Alastal, MD4
1University of Toledo College Medicine and Life Sciences, Grosse Pointe Woods, MI; 2University of Toledo, Toledo, OH; 3University of Toledo, Sylvania, OH; 4University of Toledo Medical Center, Toledo, OH
Introduction: Tuberculosis (TB) is a global health issue that affects millions of people, with gastrointestinal TB accounting for 1-3 percent of all TB cases. It often presents with nonspecific gastrointestinal (GI) symptoms, making diagnosis challenging. We present a case that highlights the clinical presentation, diagnostic journey, and management of a patient with intestinal TB presenting with findings mimicking colon cancer.
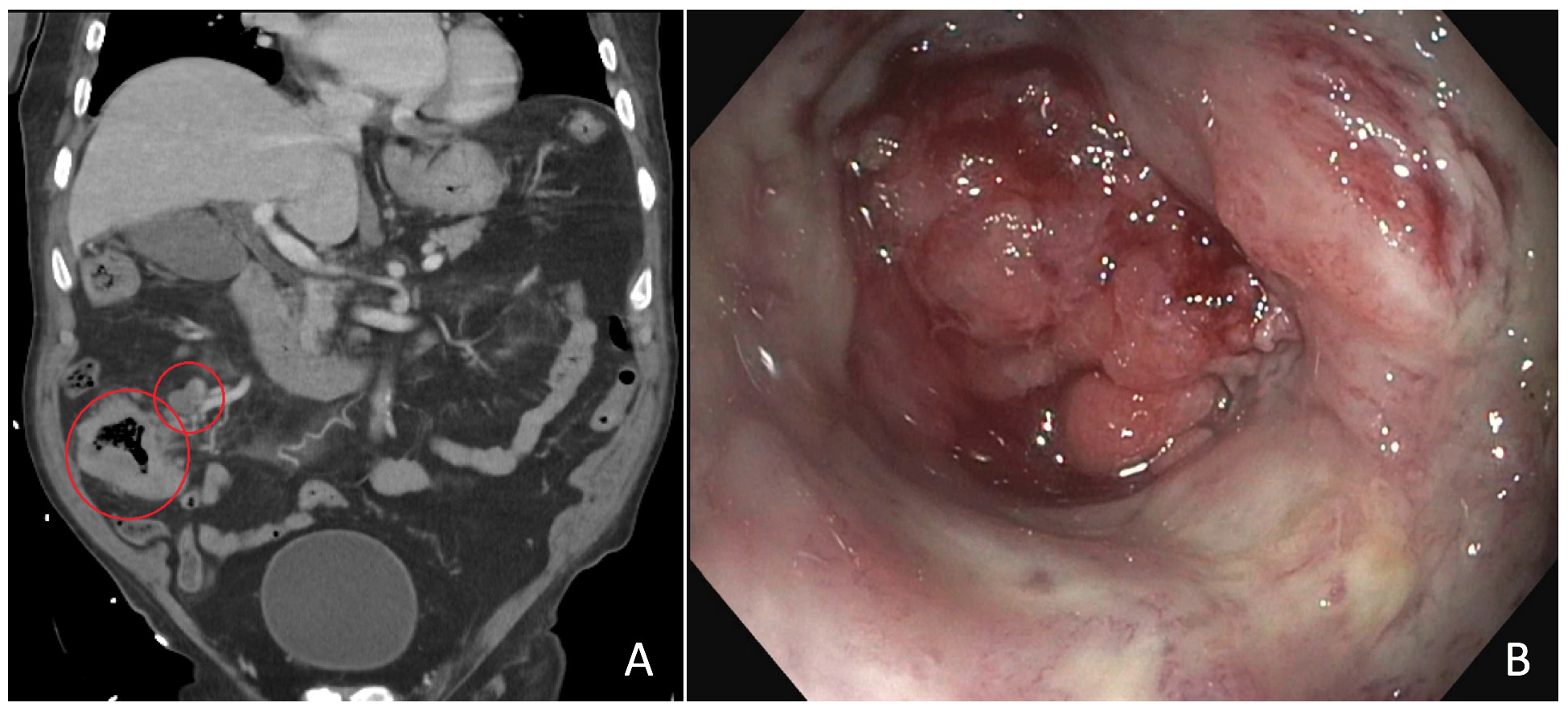
Case Description/Methods: An 85 year old male presented to the hospital for acute abdominal pain after recently being hospitalized in Mexico for a similar complaint. CT abdomen revealed circumferential mucosal wall thickening of the cecum suggestive of underlying infiltrating mass and multiple enlarged pericecal lymph nodes. A colonoscopy revealed a partially obstructing mass in the cecum. Biopsies showed colonic mucosa with ulceration and inflammatory exudate, but no evidence of malignancy. Due to high suspicion for cancer, the patient underwent a repeat colonoscopy, which showed a large ulcerative mass in the cecum that was aggressively biopsied. Biopsies revealed similar pathological changes without evidence of malignancy.
Two weeks later the patient presented with altered mentation, fevers, and hematochezia. He had COVID pneumonia. Once he returned to his baseline mentation he underwent a right colectomy with ileocolonic anastomosis. Subsequently, he had respiratory distress requiring intubation and mechanical ventilation, hemorrhagic shock on vasopressors, and an acute kidney injury resulting in hemodialysis. Eventually, the biopsy results from the surgery showed transmural necrosis, scattered necrotizing granulomas, and AFB stain revealing acid fast bacilli. The patient was diagnosed with disseminated mycobacterial infection involving the GI tract. After further goals of care discussions, he was terminally extubated.
Discussion: Intestinal TB can mimic various GI diseases, including Crohn's disease and colorectal cancer. Differentiating intestinal TB from other pathologies relies on a combination of clinical suspicion, imaging studies, endoscopic findings, and histopathological confirmation. Ascites, dual sided ileocecal involvement are usually seen in TB, and granulomas and caseating necrosis with acid-fast bacilli are indicative of TB. This case underscores the importance of considering intestinal TB in the differential diagnosis of patients presenting with findings suggestive of colon cancer, particularly in patients with relevant epidemiological exposure.
Disclosures:
Rayna Patel, MD1, Sahithi Chinnam, DO2, Sami Ghazaleh, MD3, Yaseen Alastal, MD4. P2017 - The Great Mimicker: Intestinal Tuberculosis Masquerading as Colorectal Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Toledo College Medicine and Life Sciences, Grosse Pointe Woods, MI; 2University of Toledo, Toledo, OH; 3University of Toledo, Sylvania, OH; 4University of Toledo Medical Center, Toledo, OH
Introduction: Tuberculosis (TB) is a global health issue that affects millions of people, with gastrointestinal TB accounting for 1-3 percent of all TB cases. It often presents with nonspecific gastrointestinal (GI) symptoms, making diagnosis challenging. We present a case that highlights the clinical presentation, diagnostic journey, and management of a patient with intestinal TB presenting with findings mimicking colon cancer.
Case Description/Methods: An 85 year old male presented to the hospital for acute abdominal pain after recently being hospitalized in Mexico for a similar complaint. CT abdomen revealed circumferential mucosal wall thickening of the cecum suggestive of underlying infiltrating mass and multiple enlarged pericecal lymph nodes. A colonoscopy revealed a partially obstructing mass in the cecum. Biopsies showed colonic mucosa with ulceration and inflammatory exudate, but no evidence of malignancy. Due to high suspicion for cancer, the patient underwent a repeat colonoscopy, which showed a large ulcerative mass in the cecum that was aggressively biopsied. Biopsies revealed similar pathological changes without evidence of malignancy.
Two weeks later the patient presented with altered mentation, fevers, and hematochezia. He had COVID pneumonia. Once he returned to his baseline mentation he underwent a right colectomy with ileocolonic anastomosis. Subsequently, he had respiratory distress requiring intubation and mechanical ventilation, hemorrhagic shock on vasopressors, and an acute kidney injury resulting in hemodialysis. Eventually, the biopsy results from the surgery showed transmural necrosis, scattered necrotizing granulomas, and AFB stain revealing acid fast bacilli. The patient was diagnosed with disseminated mycobacterial infection involving the GI tract. After further goals of care discussions, he was terminally extubated.
Discussion: Intestinal TB can mimic various GI diseases, including Crohn's disease and colorectal cancer. Differentiating intestinal TB from other pathologies relies on a combination of clinical suspicion, imaging studies, endoscopic findings, and histopathological confirmation. Ascites, dual sided ileocecal involvement are usually seen in TB, and granulomas and caseating necrosis with acid-fast bacilli are indicative of TB. This case underscores the importance of considering intestinal TB in the differential diagnosis of patients presenting with findings suggestive of colon cancer, particularly in patients with relevant epidemiological exposure.
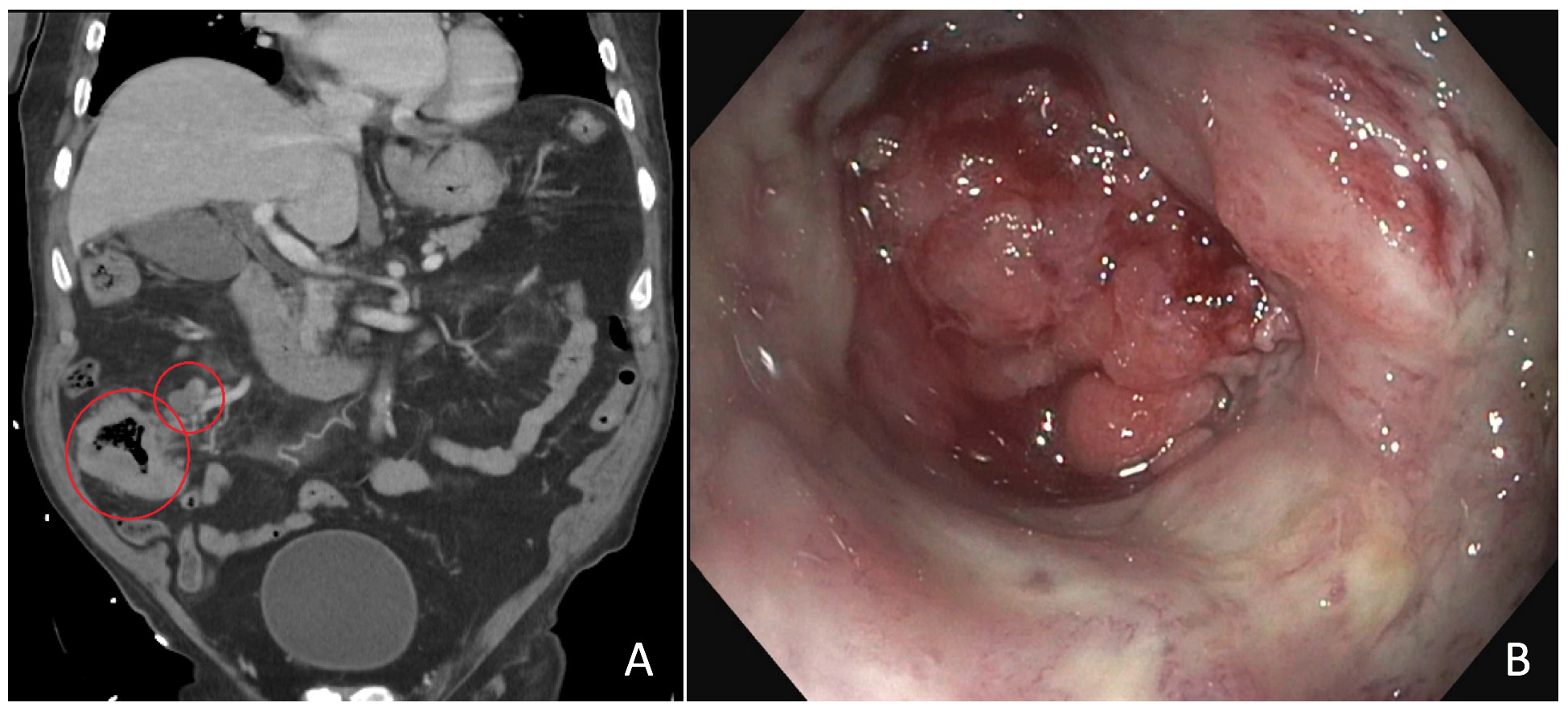
Figure: A: Computed tomography abdomen and pelvis (coronal section) showing circumferential mucosal wall thickening of the cecum with infiltrating mass (big red circle) and enlarged pericecal lymph nodes (small red circle).
B: Photograph taken at the time of the first colonoscopy showing infiltrative, partially obstructive large mass found in the cecum.
B: Photograph taken at the time of the first colonoscopy showing infiltrative, partially obstructive large mass found in the cecum.
Disclosures:
Rayna Patel indicated no relevant financial relationships.
Sahithi Chinnam indicated no relevant financial relationships.
Sami Ghazaleh indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Rayna Patel, MD1, Sahithi Chinnam, DO2, Sami Ghazaleh, MD3, Yaseen Alastal, MD4. P2017 - The Great Mimicker: Intestinal Tuberculosis Masquerading as Colorectal Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
