Monday Poster Session
Category: Biliary/Pancreas
P1870 - Postcholecystectomic Pseudoaneurysmatic Hemobilia Causing Acute Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Adily N. Elmi, MD, MPH
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Adily Elmi, MD, MPH1, Sami Mesgun, MD1, Arthur Baluyut, MD, PhD2
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Northside Gastroenterology of Indianapolis, Indianapolis, IN
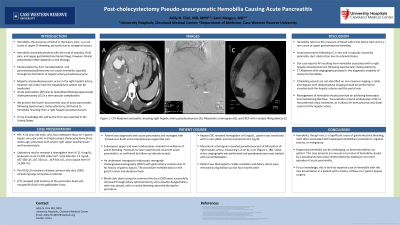
Introduction: Globally, only a few documented cases of acute pancreatitis (AP) due to hemobilia from a hepatic pseudoaneurysm (PA) following laparoscopic cholecystectomy (LC) exist. This case marks the first reported instance in the United States.
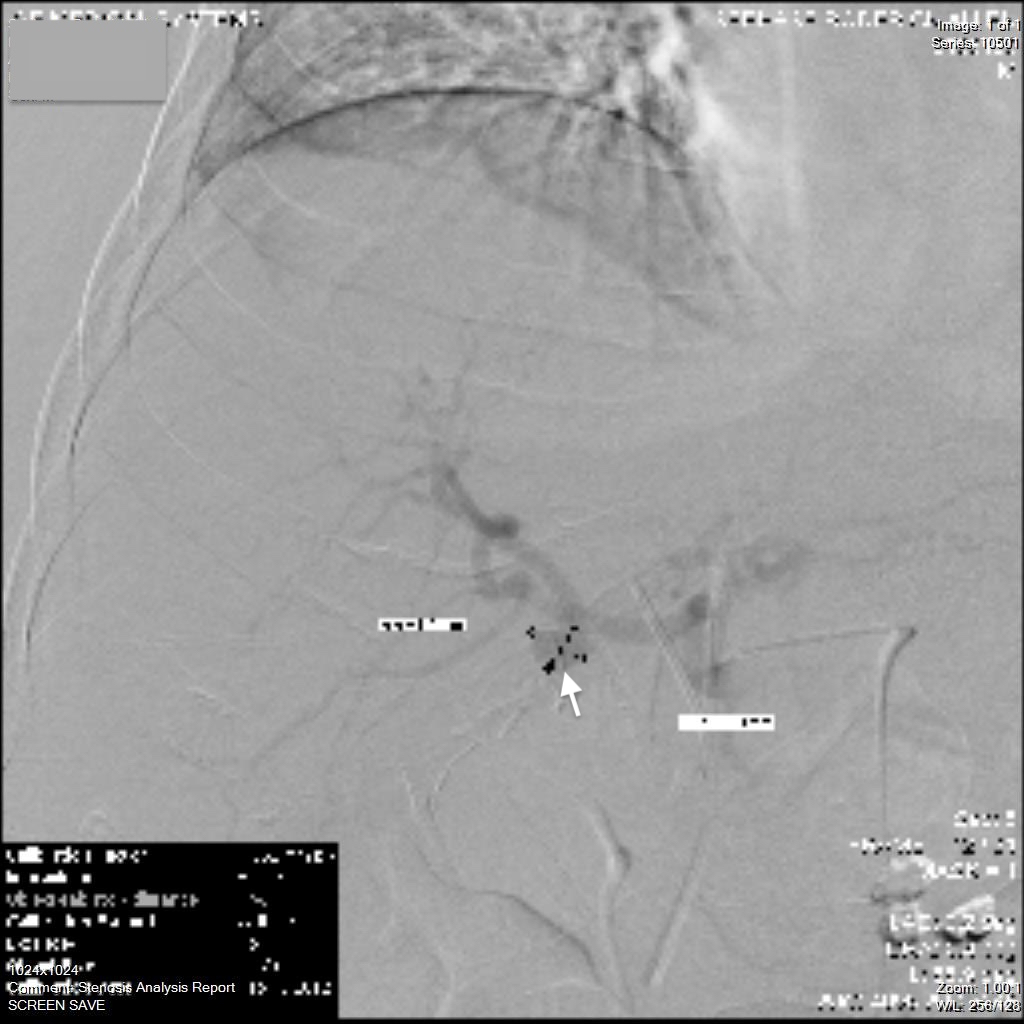
Case Description/Methods: A 56-year-old male, who underwent Roux-en-Y gastric bypass one year ago and LC three weeks ago, presented with severe RUQ pain and hematochezia. Labs showed hemoglobin 11.4 mg/dL, leukocytes 15,000 cells/mm3, total bilirubin 2.5 mg/dL, AST 638 U/L, ALT 564 U/L, ALP 814 U/L, and lipase 15,904 U/L. RUQ ultrasound demonstrated a dilated common bile duct (CBD) with large amorphous material. Abdominal computed tomography (CT) revealed mild haziness of the pancreatic head and nonspecific fluid in the gallbladder fossa. He was diagnosed with AP and managed with intravenous fluids and supportive care. Subsequent upper and lower endoscopies found no evidence of active bleeding. He later experienced recurrent AP, as confirmed by repeat lab tests. He underwent transgastric endoscopic retrograde cholangiopancreatography (ERCP) with gastrostomy creation given his gastric bypass history, which revealed blood in the gastric lumen and duodenal bulb, as well as blood draining in the ampulla. Blood clots obstructing the CBD were removed through biliary sphincterotomy and balloon catheter inflation, uncovering slow active bleeding. A double-flanged biliary stent was placed to stop the bleeding. A mesenteric arteriogram identified a PA at the bifurcation of the right hepatic artery, measuring 1.2 cm by 1 cm (Figure 1). Celiac artery angiography was performed to treat the PA with coil embolization. He was discharged in stable condition. His biliary stents were removed during a follow-up visit four months later, and he has been progressing well since.
Discussion: Hemobilia, characterized by bleeding into the biliary tree, is a rare complication after LC, and typically manifests around four weeks post-operation, with pseudoaneurysmatic hemobilia leading to AP being a unique late complication. Acute biliary signs with upper gastrointestinal (GI) bleeding suggests hemobilia, and AP in the context of upper GI bleeding indicates AP caused by hemobilia. CT angiography and celiac arteriogram can identify the bleeding source. ERCP offers both visualization and treatment options, while transcatheter arterial embolization is effective in achieving hemostasis in cases of hepatic artery hemobilia. Generative AI was used in the writing of this abstract.
Disclosures:
Adily Elmi, MD, MPH1, Sami Mesgun, MD1, Arthur Baluyut, MD, PhD2. P1870 - Postcholecystectomic Pseudoaneurysmatic Hemobilia Causing Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Northside Gastroenterology of Indianapolis, Indianapolis, IN
Introduction: Globally, only a few documented cases of acute pancreatitis (AP) due to hemobilia from a hepatic pseudoaneurysm (PA) following laparoscopic cholecystectomy (LC) exist. This case marks the first reported instance in the United States.
Case Description/Methods: A 56-year-old male, who underwent Roux-en-Y gastric bypass one year ago and LC three weeks ago, presented with severe RUQ pain and hematochezia. Labs showed hemoglobin 11.4 mg/dL, leukocytes 15,000 cells/mm3, total bilirubin 2.5 mg/dL, AST 638 U/L, ALT 564 U/L, ALP 814 U/L, and lipase 15,904 U/L. RUQ ultrasound demonstrated a dilated common bile duct (CBD) with large amorphous material. Abdominal computed tomography (CT) revealed mild haziness of the pancreatic head and nonspecific fluid in the gallbladder fossa. He was diagnosed with AP and managed with intravenous fluids and supportive care. Subsequent upper and lower endoscopies found no evidence of active bleeding. He later experienced recurrent AP, as confirmed by repeat lab tests. He underwent transgastric endoscopic retrograde cholangiopancreatography (ERCP) with gastrostomy creation given his gastric bypass history, which revealed blood in the gastric lumen and duodenal bulb, as well as blood draining in the ampulla. Blood clots obstructing the CBD were removed through biliary sphincterotomy and balloon catheter inflation, uncovering slow active bleeding. A double-flanged biliary stent was placed to stop the bleeding. A mesenteric arteriogram identified a PA at the bifurcation of the right hepatic artery, measuring 1.2 cm by 1 cm (Figure 1). Celiac artery angiography was performed to treat the PA with coil embolization. He was discharged in stable condition. His biliary stents were removed during a follow-up visit four months later, and he has been progressing well since.
Discussion: Hemobilia, characterized by bleeding into the biliary tree, is a rare complication after LC, and typically manifests around four weeks post-operation, with pseudoaneurysmatic hemobilia leading to AP being a unique late complication. Acute biliary signs with upper gastrointestinal (GI) bleeding suggests hemobilia, and AP in the context of upper GI bleeding indicates AP caused by hemobilia. CT angiography and celiac arteriogram can identify the bleeding source. ERCP offers both visualization and treatment options, while transcatheter arterial embolization is effective in achieving hemostasis in cases of hepatic artery hemobilia. Generative AI was used in the writing of this abstract.
Figure: Figure 1: Angiography image demonstrating the right hepatic pseudoaneurysm.
Disclosures:
Adily Elmi indicated no relevant financial relationships.
Sami Mesgun indicated no relevant financial relationships.
Arthur Baluyut indicated no relevant financial relationships.
Adily Elmi, MD, MPH1, Sami Mesgun, MD1, Arthur Baluyut, MD, PhD2. P1870 - Postcholecystectomic Pseudoaneurysmatic Hemobilia Causing Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

