Monday Poster Session
Category: Biliary/Pancreas
P1873 - Navigating Diagnostic and Therapeutic Hurdles in Infected Pancreatic Pseudocysts
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ana P. Rivera Arauz, MD
Nassau University Medical Center
Amityville, NY
Presenting Author(s)
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Kaleem Rizvon, MD, FACG3
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Pancreatic pseudocysts, encapsulated fluid collections without an epithelial lining, often complicate acute or chronic pancreatitis. Infected pseudocysts are particularly challenging due to their potential for severe systemic complications. The incidence of pancreatic pseudocysts in acute pancreatitis ranges from 10% to 20%, with infection occurring in about 10% of cases. This report describes an infected pancreatic pseudocyst in a 33-year-old woman, focusing on the clinical presentation and management.
Case Description/Methods: A 33-year-old Hispanic female presented with persistent lower left quadrant abdominal pain following a recent episode of acute pancreatitis. Her pancreatitis was attributed to hypertriglyceridemia. Despite initial treatment, she experienced ongoing pain, nausea, and vomiting. Physical examination revealed mild periumbilical pain and low-grade fever. Laboratory tests indicated mild anemia (hemoglobin 7.9 g/dL), elevated platelets (489 x 10^9/L), and hypertriglyceridemia (239 mg/dL).
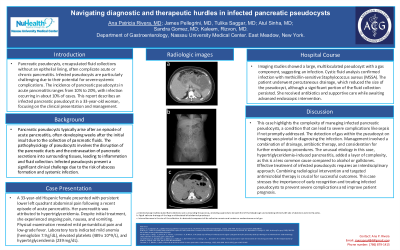
Imaging studies showed a large, multiloculated pseudocyst with a gas component, suggesting an infection. Cystic fluid analysis confirmed infection with methicillin-sensitive Staphylococcus aureus (MSSA). The patient underwent percutaneous drainage, which reduced the size of the pseudocyst, although a significant portion of the fluid collection persisted. She received antibiotics and supportive care while awaiting advanced endoscopic intervention.
Discussion: This case highlights the complexity of managing infected pancreatic pseudocysts, a condition that can lead to severe complications like sepsis if not promptly addressed. The detection of gas within the pseudocyst on imaging was pivotal in diagnosing the infection. Management involved a combination of drainage, antibiotic therapy, and consideration for further endoscopic procedures. The unusual etiology in this case, hypertriglyceridemia-induced pancreatitis, added a layer of complexity, as this is a less common cause compared to alcohol or gallstones. Effective treatment of infected pseudocysts requires an interdisciplinary approach. Combining radiological intervention and targeted antimicrobial therapy is crucial for successful outcomes. This case stresses the importance of early recognition and treating infected pseudocysts to prevent severe complications and improve patient prognosis.
Disclosures:
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Kaleem Rizvon, MD, FACG3. P1873 - Navigating Diagnostic and Therapeutic Hurdles in Infected Pancreatic Pseudocysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Pancreatic pseudocysts, encapsulated fluid collections without an epithelial lining, often complicate acute or chronic pancreatitis. Infected pseudocysts are particularly challenging due to their potential for severe systemic complications. The incidence of pancreatic pseudocysts in acute pancreatitis ranges from 10% to 20%, with infection occurring in about 10% of cases. This report describes an infected pancreatic pseudocyst in a 33-year-old woman, focusing on the clinical presentation and management.
Case Description/Methods: A 33-year-old Hispanic female presented with persistent lower left quadrant abdominal pain following a recent episode of acute pancreatitis. Her pancreatitis was attributed to hypertriglyceridemia. Despite initial treatment, she experienced ongoing pain, nausea, and vomiting. Physical examination revealed mild periumbilical pain and low-grade fever. Laboratory tests indicated mild anemia (hemoglobin 7.9 g/dL), elevated platelets (489 x 10^9/L), and hypertriglyceridemia (239 mg/dL).
Imaging studies showed a large, multiloculated pseudocyst with a gas component, suggesting an infection. Cystic fluid analysis confirmed infection with methicillin-sensitive Staphylococcus aureus (MSSA). The patient underwent percutaneous drainage, which reduced the size of the pseudocyst, although a significant portion of the fluid collection persisted. She received antibiotics and supportive care while awaiting advanced endoscopic intervention.
Discussion: This case highlights the complexity of managing infected pancreatic pseudocysts, a condition that can lead to severe complications like sepsis if not promptly addressed. The detection of gas within the pseudocyst on imaging was pivotal in diagnosing the infection. Management involved a combination of drainage, antibiotic therapy, and consideration for further endoscopic procedures. The unusual etiology in this case, hypertriglyceridemia-induced pancreatitis, added a layer of complexity, as this is a less common cause compared to alcohol or gallstones. Effective treatment of infected pseudocysts requires an interdisciplinary approach. Combining radiological intervention and targeted antimicrobial therapy is crucial for successful outcomes. This case stresses the importance of early recognition and treating infected pseudocysts to prevent severe complications and improve patient prognosis.
Disclosures:
Ana Rivera indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Tulika Saggar indicated no relevant financial relationships.
Atul Sinha indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Kaleem Rizvon, MD, FACG3. P1873 - Navigating Diagnostic and Therapeutic Hurdles in Infected Pancreatic Pseudocysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
