Monday Poster Session
Category: Biliary/Pancreas
P1877 - Challenges in Managing Choledocholelithiasis in Left Isomerism Heterotaxy Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Naresh Kumar, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Naresh Kumar, MD1, Fnu Vikash, MD, M.Med2, Sunny Kumar, MD3, Aakash Aakash, MD4, Rahul Kumar, MD5, Fnu Karishma, MBBS6, Shamsa M. Qaadri, BSc7, Amelia Panjwani, BSc7, Ruchir Damjibhai. Paladiya, MBBS8, Vikash Kumar, MD9
1The Brooklyn Hospital Center, Brooklyn, NY; 2Albert Einstein College of Medicine, New York, NY; 3The Wright Center for GME, Scranton, PA; 4Florida State University Cape Coral Hospital, Cape Coral, FL; 5Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 6Liaquat University of Medical and Health Science, Brooklyn, NY; 7St. George's University School of Medicine, Brooklyn, NY; 8University of Connecticut Health Center, Hartford, CT; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: Heterotaxy syndrome, also known as situs ambiguus, is a rare condition resulting in abnormal patterning of thoracic and abdominal organs due to embryological abnormalities. Individuals with heterotaxy syndrome face potential gastrointestinal complications, such as intestinal malrotation, biliary atresia, infections, gallstone formation, and pancreatitis. This case presentation discusses the management of choledocholelithiasis, a plausible biliary complication, in a 49-year-old male with left isomerism heterotaxy syndrome.
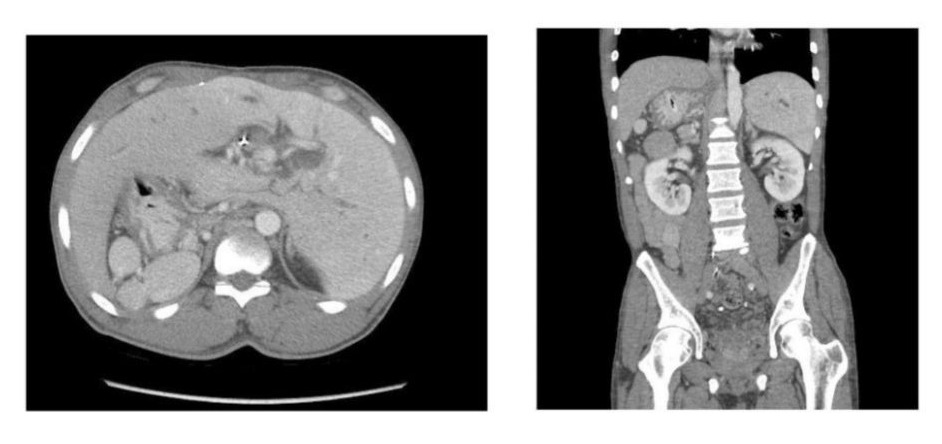
Case Description/Methods: A 49-year-old male with schizophrenia and a history of a biliary stent for a CBD stone presented with five days of abdominal pain, bilious emesis, and nausea. On admission, he was stable but had leukocytosis (12.3 K), cholestatic LFTs, and RUQ tenderness. CT revealed left isomerism heterotaxy syndrome with polysplenia, severe intrahepatic biliary dilation, multiple right biliary duct defects, and an abnormal biliary confluence. Broad spectrum antibiotics were started. ERCP showed a severely dilated CBD obstructed by a stone. The obstruction was managed with dilation, stent removal, sphincteroplasty, balloon sweeps, cholangioscopy, and lithotripsy. Post-ERCP, a duodenal bend stent normalized LFTs and WBCs. Due to the large stone burden, complex anatomy, and duodenoscope positioning challenges, the surgery team opted for laparoscopic cholecystectomy, which later converted to open surgery. They retrieved ~20 stones (some 5-8 cm) and placed a T-tube. Despite the intervention, a cholangiogram four weeks later showed recurrent distal CBD obstruction, prompting a transfer to a tertiary center for further management of his complicated anatomy.
Discussion: Heterotaxy syndrome introduces unique anatomical variations, increasing susceptibility to biliary complications.The atypical anatomy associated with this syndrome increases the vulnerability to biliary complications, including recurrent choledocholithiasis, posing significant hurdles for interventions such as endoscopic retrograde cholangiopancreatography (ERCP) and surgery. Anatomical anomalies linked to heterotaxy syndrome, such as an enlarged liver, midline gallbladder, multiple splenules, and small bowel malrotation, adds layers of complexity to the management strategy. This case underscores the complexity of managing biliary complications in heterotaxy syndrome and emphasizes the importance of tailored, multidisciplinary approaches.
Disclosures:
Naresh Kumar, MD1, Fnu Vikash, MD, M.Med2, Sunny Kumar, MD3, Aakash Aakash, MD4, Rahul Kumar, MD5, Fnu Karishma, MBBS6, Shamsa M. Qaadri, BSc7, Amelia Panjwani, BSc7, Ruchir Damjibhai. Paladiya, MBBS8, Vikash Kumar, MD9. P1877 - Challenges in Managing Choledocholelithiasis in Left Isomerism Heterotaxy Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Brooklyn Hospital Center, Brooklyn, NY; 2Albert Einstein College of Medicine, New York, NY; 3The Wright Center for GME, Scranton, PA; 4Florida State University Cape Coral Hospital, Cape Coral, FL; 5Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 6Liaquat University of Medical and Health Science, Brooklyn, NY; 7St. George's University School of Medicine, Brooklyn, NY; 8University of Connecticut Health Center, Hartford, CT; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: Heterotaxy syndrome, also known as situs ambiguus, is a rare condition resulting in abnormal patterning of thoracic and abdominal organs due to embryological abnormalities. Individuals with heterotaxy syndrome face potential gastrointestinal complications, such as intestinal malrotation, biliary atresia, infections, gallstone formation, and pancreatitis. This case presentation discusses the management of choledocholelithiasis, a plausible biliary complication, in a 49-year-old male with left isomerism heterotaxy syndrome.
Case Description/Methods: A 49-year-old male with schizophrenia and a history of a biliary stent for a CBD stone presented with five days of abdominal pain, bilious emesis, and nausea. On admission, he was stable but had leukocytosis (12.3 K), cholestatic LFTs, and RUQ tenderness. CT revealed left isomerism heterotaxy syndrome with polysplenia, severe intrahepatic biliary dilation, multiple right biliary duct defects, and an abnormal biliary confluence. Broad spectrum antibiotics were started. ERCP showed a severely dilated CBD obstructed by a stone. The obstruction was managed with dilation, stent removal, sphincteroplasty, balloon sweeps, cholangioscopy, and lithotripsy. Post-ERCP, a duodenal bend stent normalized LFTs and WBCs. Due to the large stone burden, complex anatomy, and duodenoscope positioning challenges, the surgery team opted for laparoscopic cholecystectomy, which later converted to open surgery. They retrieved ~20 stones (some 5-8 cm) and placed a T-tube. Despite the intervention, a cholangiogram four weeks later showed recurrent distal CBD obstruction, prompting a transfer to a tertiary center for further management of his complicated anatomy.
Discussion: Heterotaxy syndrome introduces unique anatomical variations, increasing susceptibility to biliary complications.The atypical anatomy associated with this syndrome increases the vulnerability to biliary complications, including recurrent choledocholithiasis, posing significant hurdles for interventions such as endoscopic retrograde cholangiopancreatography (ERCP) and surgery. Anatomical anomalies linked to heterotaxy syndrome, such as an enlarged liver, midline gallbladder, multiple splenules, and small bowel malrotation, adds layers of complexity to the management strategy. This case underscores the complexity of managing biliary complications in heterotaxy syndrome and emphasizes the importance of tailored, multidisciplinary approaches.
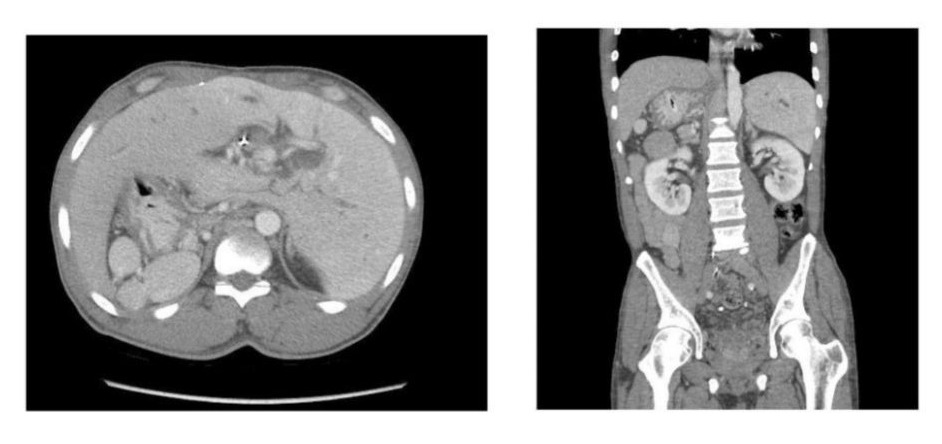
Figure: CT scan of abdomen and pelvis with contrast showing enlarged liver with gallbladder in the midline position and multiple splenules.
Disclosures:
Naresh Kumar indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Aakash Aakash indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Fnu Karishma indicated no relevant financial relationships.
Shamsa Qaadri indicated no relevant financial relationships.
Amelia Panjwani indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Naresh Kumar, MD1, Fnu Vikash, MD, M.Med2, Sunny Kumar, MD3, Aakash Aakash, MD4, Rahul Kumar, MD5, Fnu Karishma, MBBS6, Shamsa M. Qaadri, BSc7, Amelia Panjwani, BSc7, Ruchir Damjibhai. Paladiya, MBBS8, Vikash Kumar, MD9. P1877 - Challenges in Managing Choledocholelithiasis in Left Isomerism Heterotaxy Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
