Monday Poster Session
Category: Biliary/Pancreas
P1882 - A Rare Case of Autoimmune Pancreatitis Mimicking Pancreatic Cancer
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MI
Muhammad Ismail, MD
Indiana University Southwest
Cedar Rapids, IA
Presenting Author(s)
Muhammad Ismail, MD1, Muhammad Chaudhary, MBChB2, Oluwagbenga Serrano, MD, FACG3
1Indiana University School of Medicine Southwest, Cedar Rapids, IA; 2Indiana University School of Medicine Southwest, Evansville, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Autoimmune pancreatitis (AIP) is a rare inflammatory condition characterized by pancreatic enlargement, irregular narrowing of the pancreatic duct, and elevated serum IgG4 levels. Its clinical and radiological resemblance to pancreatic cancer poses significant diagnostic challenges. Distinguishing AIP from pancreatic malignancy is critical to avoid unnecessary surgical interventions and initiate appropriate treatment. We present a case of AIP initially misdiagnosed as pancreatic cancer, underscoring the importance of thorough evaluation in atypical presentations.
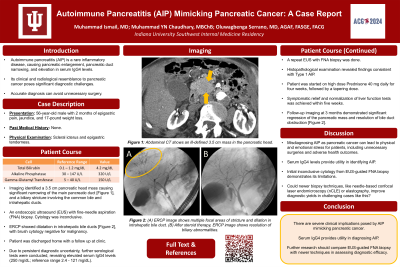
Case Description/Methods: A 56-year-old male presented with a two-month history of epigastric pain, jaundice, and a 17-pound weight loss. Physical examination revealed icteric sclera and epigastric tenderness. Laboratory investigations showed elevated serum bilirubin (4.2 mg/dL), alkaline phosphatase (320 U/L), and gamma-glutamyl transferase (150 U/L). Contrast-enhanced CT and MRI of the abdomen identified a 3.5 cm pancreatic head mass causing significant narrowing of the main pancreatic duct. Additionally, a 3 cm biliary stricture involving the common bile duct and intrahepatic ducts, was identified, contributing to the marked jaundice observed in the patient.
Endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) biopsy was performed, but cytology was inconclusive. ERCP with brush cytology also failed to confirm malignancy. Due to persistent diagnostic uncertainty, further serological tests were conducted, revealing elevated serum IgG4 levels (250 mg/dL).
A repeat EUS-guided FNA biopsy with histopathological examination revealed dense lymphoplasmacytic infiltration and storiform fibrosis, consistent with type 1 AIP. The patient was commenced on prednisone 40 mg daily for four weeks, followed by a tapering dose. Symptomatic relief and normalization of liver function tests was achieved within five weeks. Follow-up imaging at three months demonstrated significant regression of the pancreatic mass and resolution of bile duct obstruction, confirming the diagnosis of AIP.
Discussion: This case highlights the challenges posed by AIP mimicking pancreatic cancer, given the stark contrast in management and prognosis. AIP should be considered in the differential diagnosis of pancreatic masses. Misdiagnosis can lead to unnecessary surgical resections. EUS-guided FNA biopsy and serum IgG4 provides utility in diagnosing AIP. Prompt steroid therapy can induce remission, as demonstrated in our patient, highlighting its therapeutic efficacy.
Disclosures:
Muhammad Ismail, MD1, Muhammad Chaudhary, MBChB2, Oluwagbenga Serrano, MD, FACG3. P1882 - A Rare Case of Autoimmune Pancreatitis Mimicking Pancreatic Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine Southwest, Cedar Rapids, IA; 2Indiana University School of Medicine Southwest, Evansville, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Autoimmune pancreatitis (AIP) is a rare inflammatory condition characterized by pancreatic enlargement, irregular narrowing of the pancreatic duct, and elevated serum IgG4 levels. Its clinical and radiological resemblance to pancreatic cancer poses significant diagnostic challenges. Distinguishing AIP from pancreatic malignancy is critical to avoid unnecessary surgical interventions and initiate appropriate treatment. We present a case of AIP initially misdiagnosed as pancreatic cancer, underscoring the importance of thorough evaluation in atypical presentations.
Case Description/Methods: A 56-year-old male presented with a two-month history of epigastric pain, jaundice, and a 17-pound weight loss. Physical examination revealed icteric sclera and epigastric tenderness. Laboratory investigations showed elevated serum bilirubin (4.2 mg/dL), alkaline phosphatase (320 U/L), and gamma-glutamyl transferase (150 U/L). Contrast-enhanced CT and MRI of the abdomen identified a 3.5 cm pancreatic head mass causing significant narrowing of the main pancreatic duct. Additionally, a 3 cm biliary stricture involving the common bile duct and intrahepatic ducts, was identified, contributing to the marked jaundice observed in the patient.
Endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) biopsy was performed, but cytology was inconclusive. ERCP with brush cytology also failed to confirm malignancy. Due to persistent diagnostic uncertainty, further serological tests were conducted, revealing elevated serum IgG4 levels (250 mg/dL).
A repeat EUS-guided FNA biopsy with histopathological examination revealed dense lymphoplasmacytic infiltration and storiform fibrosis, consistent with type 1 AIP. The patient was commenced on prednisone 40 mg daily for four weeks, followed by a tapering dose. Symptomatic relief and normalization of liver function tests was achieved within five weeks. Follow-up imaging at three months demonstrated significant regression of the pancreatic mass and resolution of bile duct obstruction, confirming the diagnosis of AIP.
Discussion: This case highlights the challenges posed by AIP mimicking pancreatic cancer, given the stark contrast in management and prognosis. AIP should be considered in the differential diagnosis of pancreatic masses. Misdiagnosis can lead to unnecessary surgical resections. EUS-guided FNA biopsy and serum IgG4 provides utility in diagnosing AIP. Prompt steroid therapy can induce remission, as demonstrated in our patient, highlighting its therapeutic efficacy.
Disclosures:
Muhammad Ismail indicated no relevant financial relationships.
Muhammad Chaudhary indicated no relevant financial relationships.
Oluwagbenga Serrano: MERCK – Stock-publicly held company(excluding mutual/index funds).
Muhammad Ismail, MD1, Muhammad Chaudhary, MBChB2, Oluwagbenga Serrano, MD, FACG3. P1882 - A Rare Case of Autoimmune Pancreatitis Mimicking Pancreatic Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
