Monday Poster Session
Category: Biliary/Pancreas
P1788 - Vanishing Bile Duct Syndrome Resulting From HIV Viremia: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael J. DiMarino, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Michael J. DiMarino, MD1, Emily Chiacchiaro, MD1, Kevan Josloff, MD, MPH1, Akash Patel, DO1, Beatriz Torre, MD2, Benjamin Young, MD1, Rebecca Loh, MD1, Steven Herrine, MD3
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Vanishing bile duct syndrome (VBDS) is defined by loss of small and medium sized intrahepatic bile ducts most commonly associated with drug-induced liver injury. VBDS associated with uncontrolled human immunodeficiency virus (HIV) infection has rarely been reported.1 We herein report a patient with HIV-associated, histologically proven VBDS.
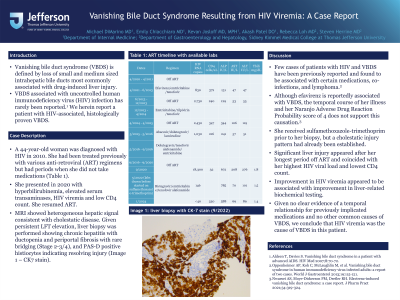
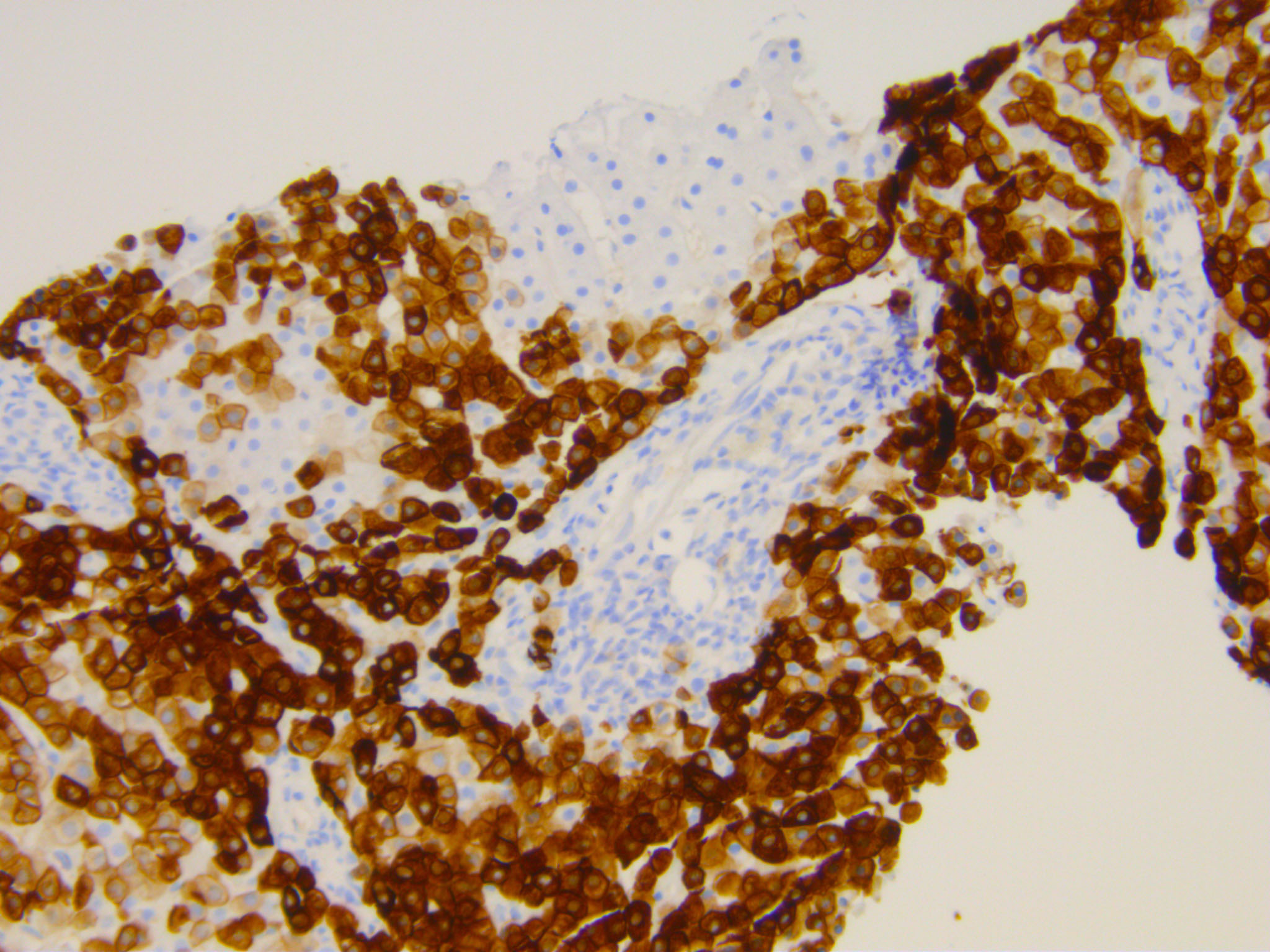
Case Description/Methods: A 44-year-old woman was diagnosed with HIV in 2010. She had been treated previously with various anti-retroviral (ART) regimens but had periods when she did not take medications (Table 1). She presented in 2020 with hyperbilirubinemia, elevated serum transaminases, HIV viremia and low CD4 count. She resumed ART. MRI showed heterogeneous hepatic signal consistent with cholestatic disease. Given persistent LFT elevation, liver biopsy was performed showing chronic hepatitis with ductopenia and periportal fibrosis with rare bridging (Stage 2-3/4), and PAS-D positive histiocytes indicating resolving injury (Image 1).
Discussion: Few cases of patients with HIV and VBDS have been previously reported and found to be associated with certain medications, co-infections, and lymphoma.2 Although Efavirenz is reportedly associated with VBDS, the temporal course of her illness and her Naranjo Adverse Drug Reaction Probability score of 4 does not support this causation.3 She received sulfamethoxazole-trimethoprim prior to her biopsy, but a cholestatic injury pattern had already been established. Significant liver injury appeared after her longest period off ART and coincided with her highest HIV viral load and lowest CD4 count. Improvement in HIV viremia appeared to be associated with improvement in liver-related biochemical testing. Given no clear evidence of a temporal relationship for previously implicated medications and no other common causes of VBDS, we conclude that HIV viremia was the cause of VBDS in this patient.
1. Aldeen T, Davies S. Vanishing bile duct syndrome in a patient with advanced AIDS. HIV Med 2007;8:70-72.
2. Oppenheimer AP, Koh C, McLaughlin M, et al. Vanishing bile duct syndrome in human immunodeficiency virus infected adults: A report of two cases. World J Gastroenterol 2013;19:115-121.
3. Nwaesei AS, Moy-Dickerson PM, Dretler RH. Efavirenz-induced vanishing bile duct syndrome: a case report. J Pharm Pract 2021;34:319-324.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael J. DiMarino, MD1, Emily Chiacchiaro, MD1, Kevan Josloff, MD, MPH1, Akash Patel, DO1, Beatriz Torre, MD2, Benjamin Young, MD1, Rebecca Loh, MD1, Steven Herrine, MD3. P1788 - Vanishing Bile Duct Syndrome Resulting From HIV Viremia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Vanishing bile duct syndrome (VBDS) is defined by loss of small and medium sized intrahepatic bile ducts most commonly associated with drug-induced liver injury. VBDS associated with uncontrolled human immunodeficiency virus (HIV) infection has rarely been reported.1 We herein report a patient with HIV-associated, histologically proven VBDS.
Case Description/Methods: A 44-year-old woman was diagnosed with HIV in 2010. She had been treated previously with various anti-retroviral (ART) regimens but had periods when she did not take medications (Table 1). She presented in 2020 with hyperbilirubinemia, elevated serum transaminases, HIV viremia and low CD4 count. She resumed ART. MRI showed heterogeneous hepatic signal consistent with cholestatic disease. Given persistent LFT elevation, liver biopsy was performed showing chronic hepatitis with ductopenia and periportal fibrosis with rare bridging (Stage 2-3/4), and PAS-D positive histiocytes indicating resolving injury (Image 1).
Discussion: Few cases of patients with HIV and VBDS have been previously reported and found to be associated with certain medications, co-infections, and lymphoma.2 Although Efavirenz is reportedly associated with VBDS, the temporal course of her illness and her Naranjo Adverse Drug Reaction Probability score of 4 does not support this causation.3 She received sulfamethoxazole-trimethoprim prior to her biopsy, but a cholestatic injury pattern had already been established. Significant liver injury appeared after her longest period off ART and coincided with her highest HIV viral load and lowest CD4 count. Improvement in HIV viremia appeared to be associated with improvement in liver-related biochemical testing. Given no clear evidence of a temporal relationship for previously implicated medications and no other common causes of VBDS, we conclude that HIV viremia was the cause of VBDS in this patient.
1. Aldeen T, Davies S. Vanishing bile duct syndrome in a patient with advanced AIDS. HIV Med 2007;8:70-72.
2. Oppenheimer AP, Koh C, McLaughlin M, et al. Vanishing bile duct syndrome in human immunodeficiency virus infected adults: A report of two cases. World J Gastroenterol 2013;19:115-121.
3. Nwaesei AS, Moy-Dickerson PM, Dretler RH. Efavirenz-induced vanishing bile duct syndrome: a case report. J Pharm Pract 2021;34:319-324.
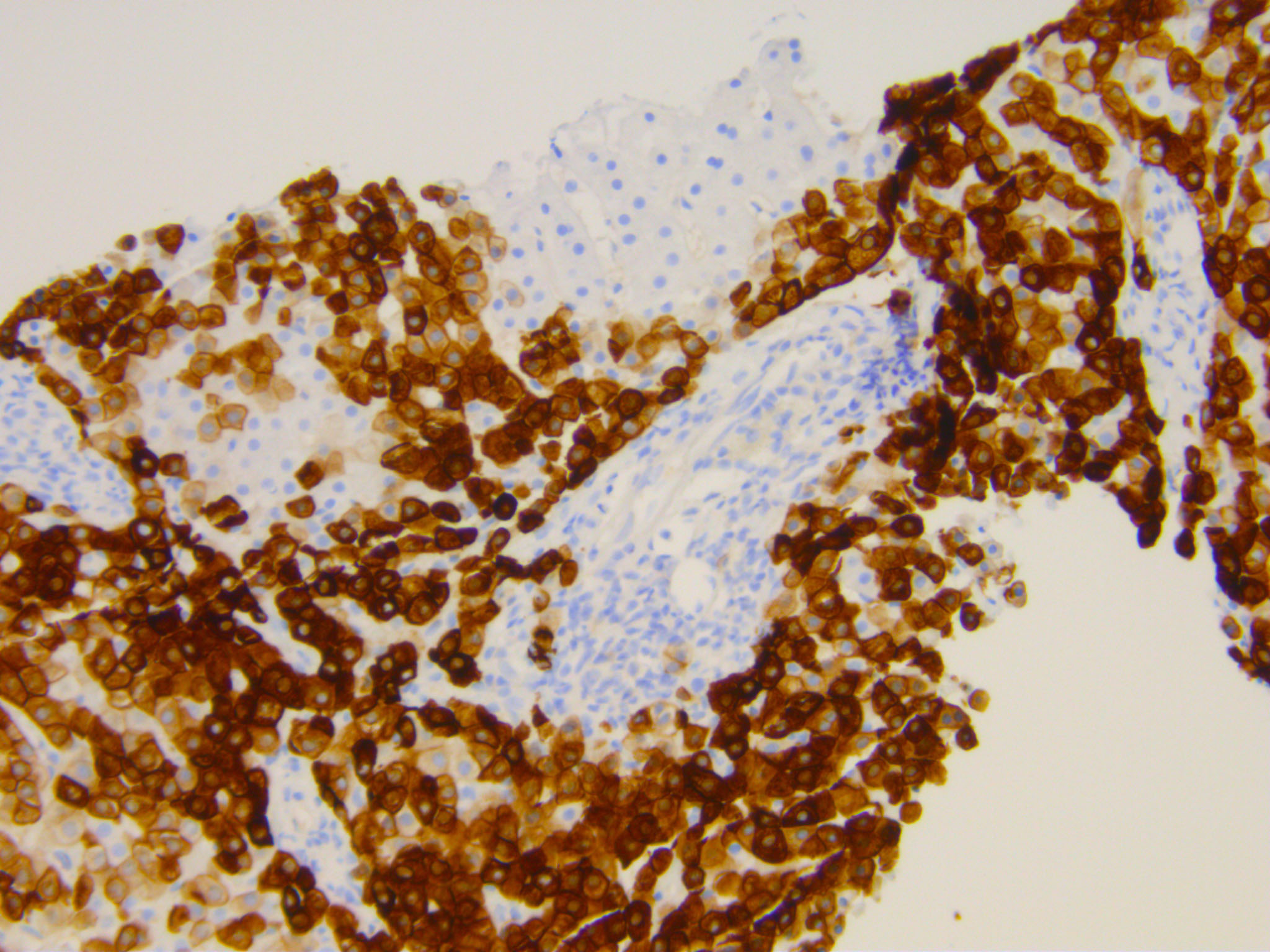
Figure: Attached is a photomicrograph of patient's liver biopsy with Cytokeratin 7 stain. It shows a portal tract devoid of a bile duct.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael DiMarino indicated no relevant financial relationships.
Emily Chiacchiaro indicated no relevant financial relationships.
Kevan Josloff indicated no relevant financial relationships.
Akash Patel indicated no relevant financial relationships.
Beatriz Torre indicated no relevant financial relationships.
Benjamin Young indicated no relevant financial relationships.
Rebecca Loh indicated no relevant financial relationships.
Steven Herrine indicated no relevant financial relationships.
Michael J. DiMarino, MD1, Emily Chiacchiaro, MD1, Kevan Josloff, MD, MPH1, Akash Patel, DO1, Beatriz Torre, MD2, Benjamin Young, MD1, Rebecca Loh, MD1, Steven Herrine, MD3. P1788 - Vanishing Bile Duct Syndrome Resulting From HIV Viremia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
