Sunday Poster Session
Category: Stomach
P1697 - Emphysematous Esophagitis and Gastritis in a Critically Ill Diabetic Patient Undergoing Intrapleural tPA-DNase Therapy: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Mohammed Rifat Shaik, MBBS
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Akshay Duddu, MD4, Aleksan Khachatryan, MD1
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2SSM Health/Saint Louis University School of Medicine, St. Louis, MO; 3University of Maryland Capital Region Health, Lorton, VA; 4Greater Baltimore Medical Center, Towson, MD
Introduction: Emphysematous gastritis (EG) is a rare type of gastritis caused by gas-producing infectious organisms. We present a case of EG in a critically ill diabetic patient with sepsis who was undergoing intrapleural alteplase-dornase (tPA + DNase) therapy.
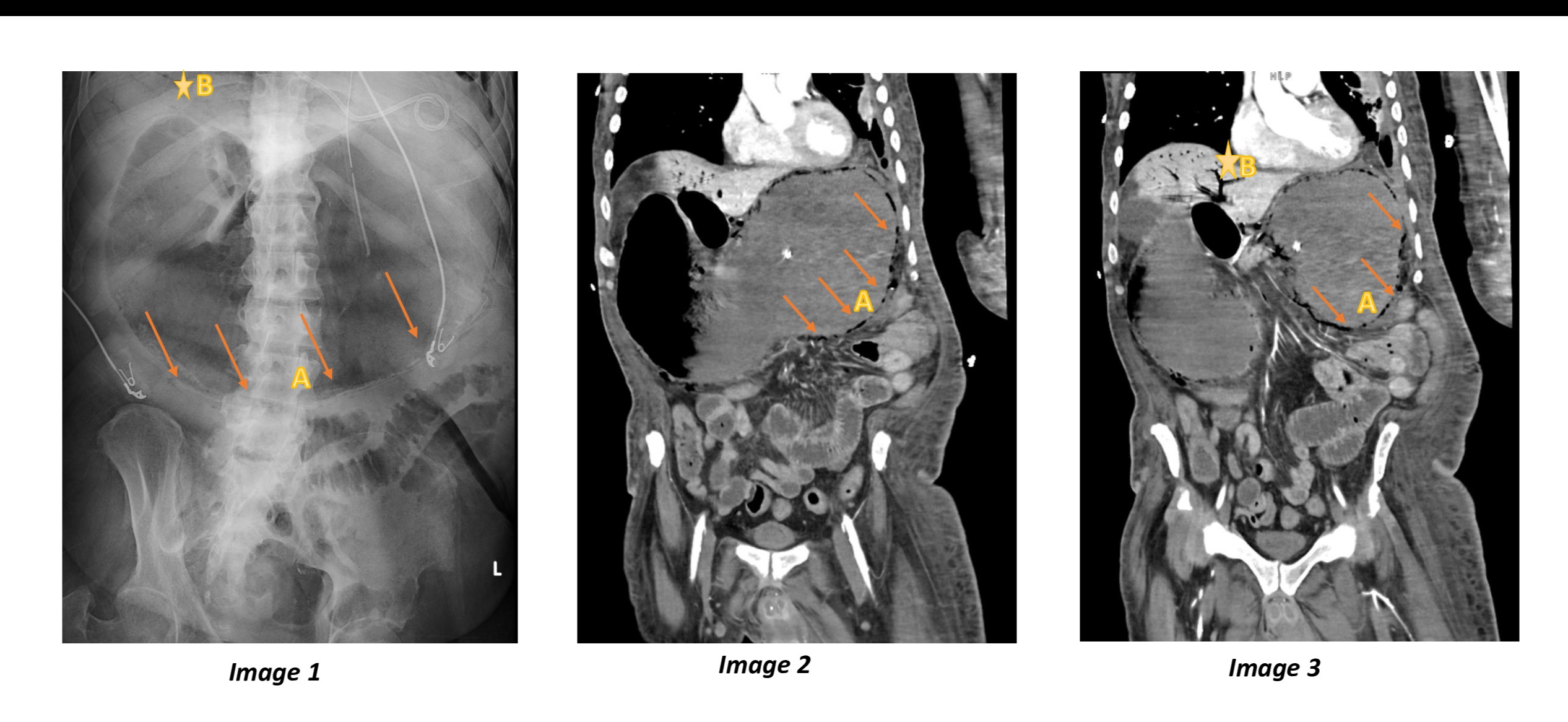
Case Description/Methods: A 60-year-old male with a history of diabetes mellitus (DM) and end-stage renal disease on hemodialysis presented with sepsis from wet gangrene of the right foot and an infected sacral decubitus ulcer. He was placed on broad-spectrum antibiotics and underwent source control, including sacral ulcer debridement and partial first-ray amputation of right foot. Blood cultures were negative. However, persistent hypotension prompted a computed tomography (CT) scan of the chest and abdomen, which revealed a left lower lung opacity with loculated pleural effusion concerning for empyema. A chest tube was placed with minimal drainage. Multiple doses of intrapleural tPA + DNase were given. The patient subsequently developed status epilepticus, requiring intubation and nasogastric (NG) tube placement. He required vasopressor support and continued broad-spectrum antibiotic coverage. His condition was further complicated by abdominal distension and worsening leukocytosis. Evaluation with abdominal imaging, including radiograph and CT, showed gastric distention with gastric and esophageal pneumatosis and portal venous gas. tPA + DNase therapy was withheld. The NG tube was set to continuous suction. Micafungin was added for fungal coverage. He was deemed to be a poor surgical candidate and was transitioned to comfort care.
Discussion: Our patient had predisposing factors for EG, including DM and renal failure. Recent tPA/dornase therapy and NG tube insertion may have further compromised the gastric mucosal barrier. In this critically ill patient with sepsis, bacterial invasion of the breached mucosa may have led to intramural gas formation and subsequent translocation into the portal veins and liver. Diagnosis relied on CT imaging demonstrating streaky and linear intramural gas and gastric wall thickening. Treatment involved conservative measures such as broad-spectrum antibiotics and bowel rest. Since Candida species and polymicrobial infections are common, empirical antifungal therapy was added pending further testing. Surgical intervention was not pursued due to multiple active conditions, poor overall prognosis, and absence of complications such as perforation.
Disclosures:
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Akshay Duddu, MD4, Aleksan Khachatryan, MD1. P1697 - Emphysematous Esophagitis and Gastritis in a Critically Ill Diabetic Patient Undergoing Intrapleural tPA-DNase Therapy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2SSM Health/Saint Louis University School of Medicine, St. Louis, MO; 3University of Maryland Capital Region Health, Lorton, VA; 4Greater Baltimore Medical Center, Towson, MD
Introduction: Emphysematous gastritis (EG) is a rare type of gastritis caused by gas-producing infectious organisms. We present a case of EG in a critically ill diabetic patient with sepsis who was undergoing intrapleural alteplase-dornase (tPA + DNase) therapy.
Case Description/Methods: A 60-year-old male with a history of diabetes mellitus (DM) and end-stage renal disease on hemodialysis presented with sepsis from wet gangrene of the right foot and an infected sacral decubitus ulcer. He was placed on broad-spectrum antibiotics and underwent source control, including sacral ulcer debridement and partial first-ray amputation of right foot. Blood cultures were negative. However, persistent hypotension prompted a computed tomography (CT) scan of the chest and abdomen, which revealed a left lower lung opacity with loculated pleural effusion concerning for empyema. A chest tube was placed with minimal drainage. Multiple doses of intrapleural tPA + DNase were given. The patient subsequently developed status epilepticus, requiring intubation and nasogastric (NG) tube placement. He required vasopressor support and continued broad-spectrum antibiotic coverage. His condition was further complicated by abdominal distension and worsening leukocytosis. Evaluation with abdominal imaging, including radiograph and CT, showed gastric distention with gastric and esophageal pneumatosis and portal venous gas. tPA + DNase therapy was withheld. The NG tube was set to continuous suction. Micafungin was added for fungal coverage. He was deemed to be a poor surgical candidate and was transitioned to comfort care.
Discussion: Our patient had predisposing factors for EG, including DM and renal failure. Recent tPA/dornase therapy and NG tube insertion may have further compromised the gastric mucosal barrier. In this critically ill patient with sepsis, bacterial invasion of the breached mucosa may have led to intramural gas formation and subsequent translocation into the portal veins and liver. Diagnosis relied on CT imaging demonstrating streaky and linear intramural gas and gastric wall thickening. Treatment involved conservative measures such as broad-spectrum antibiotics and bowel rest. Since Candida species and polymicrobial infections are common, empirical antifungal therapy was added pending further testing. Surgical intervention was not pursued due to multiple active conditions, poor overall prognosis, and absence of complications such as perforation.
Figure: Image 1 is an abdominal X-ray revealing distal esophageal and gastric pneumatosis (arrows, A) with gastric distention and portal venous gas (star, B). Images 2 and 3 are coronal CT scans of the abdomen showing gastric and esophageal pneumatosis (indicated by arrows, A) along with significant gastric distention. Additionally, portal venous gas is noted (marked by the star, B).
Disclosures:
Mohammed Rifat Shaik indicated no relevant financial relationships.
Nishat Anjum Shaik indicated no relevant financial relationships.
Zainab Mujahid indicated no relevant financial relationships.
Akshay Duddu indicated no relevant financial relationships.
Aleksan Khachatryan indicated no relevant financial relationships.
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Akshay Duddu, MD4, Aleksan Khachatryan, MD1. P1697 - Emphysematous Esophagitis and Gastritis in a Critically Ill Diabetic Patient Undergoing Intrapleural tPA-DNase Therapy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
