Sunday Poster Session
Category: Stomach
P1703 - Disseminated Tuberculosis with Gastrointestinal and Splenic Involvement masquerading as Metastatic Malignancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Theja Channapragada, DO, MBA, MS
Penn State Health Milton S. Hershey Medical Center
Springfield, NJ
Presenting Author(s)
Theja Channapragada, DO, MBA, MS1, Abirami Rajendiran, MD2, Arkady Broder, MD3, Jonathan Nunez, MD4, Srinivas Channapragada, MD5
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 5Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Springfield, NJ
Introduction: Gastrointestinal Tuberculosis (GITB) is infrequent in developed nations but accounts for 12% of extrapulmonary tuberculosis(TB) cases. Splenic TB(STB) is seldom reported. Specific populations in the US are at higher risk for TB. These include immigrants from developing countries, individuals with weakened immune systems such as the elderly, diabetics, and those who are HIV-positive, as well as incarcerated individuals. Despite the widely known prevalence of pulmonary TB, GITB and STB can be mistaken for malignancy. For patients presenting with upper abdominal complaints and weight loss, the diagnosis of TB should be ruled out.
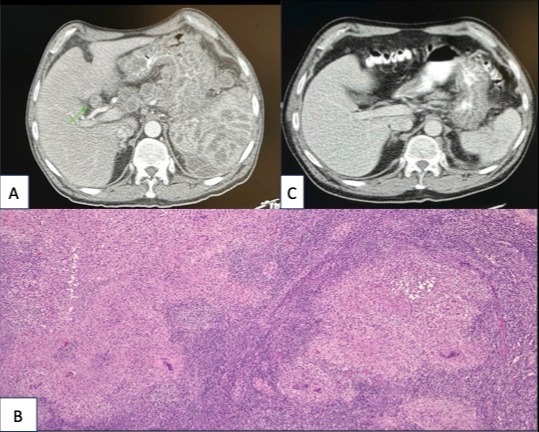
Case Description/Methods: A 66-year-old male from Nicaragua presented with a 60-lb weight loss, decreased appetite, and epigastric pain. The patient's mother died of gastric cancer. He denied history of tobacco or alcohol use. Tuberculin skin testing (TST), HIV, and interferon-gamma release assay (IGRA) were negative. Esophagogastroduodenoscopy(EGD) showed diffuse ulcerated thickened gastric folds with negative gastric mucosal biopsies. Computed Tomography Abdomen and Pelvis (CT A/P) with contrast revealed multiple enlarged intraabdominal lymph nodes, irregular thickening of the gastric mucosa, and innumerable hypodense splenic lesions(A). Endoscopic Ultrasound (EUS) with fine needle aspiration biopsy (FNAB) of intraabdominal lymph nodes showed scant fibrinopurulent material that was Acid-fast bacteria (AFB) negative. Flow cytometry was unremarkable. Biopsy of axillary lymph nodes showed caseating granulomas(B). The patient was diagnosed with disseminated TB involving the stomach and spleen. Anti-TB therapy led to symptom resolution and weight gain in six months(C).
Discussion: The incidence of TB in Nicaragua (45/100,000) is higher than in the USA, which is (3/100,000). The diagnosis of GI TB mimics other conditions such as inflammatory bowel disease, peptic ulcer disease, or malignancy. Isolated splenic TB can present with jaundice and hepatosplenomegaly. While TST and IGRA are frequently positive in patients with GITB and STB, a negative TST or IGRA does not rule out active TB. The sensitivity for detecting GI TB through AFB with upper EGD with tissue sampling through biopsy or mucosal resection is low. FNAB may reach the deeper submucosa more effectively to locate caseating granulomas/acid-fast bacillus. STB may reveal hypodense splenic lesions on CT A/P. The recommended treatment for GITB and STB is a regimen of anti-TB therapy.
Disclosures:
Theja Channapragada, DO, MBA, MS1, Abirami Rajendiran, MD2, Arkady Broder, MD3, Jonathan Nunez, MD4, Srinivas Channapragada, MD5. P1703 - Disseminated Tuberculosis with Gastrointestinal and Splenic Involvement masquerading as Metastatic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 5Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Springfield, NJ
Introduction: Gastrointestinal Tuberculosis (GITB) is infrequent in developed nations but accounts for 12% of extrapulmonary tuberculosis(TB) cases. Splenic TB(STB) is seldom reported. Specific populations in the US are at higher risk for TB. These include immigrants from developing countries, individuals with weakened immune systems such as the elderly, diabetics, and those who are HIV-positive, as well as incarcerated individuals. Despite the widely known prevalence of pulmonary TB, GITB and STB can be mistaken for malignancy. For patients presenting with upper abdominal complaints and weight loss, the diagnosis of TB should be ruled out.
Case Description/Methods: A 66-year-old male from Nicaragua presented with a 60-lb weight loss, decreased appetite, and epigastric pain. The patient's mother died of gastric cancer. He denied history of tobacco or alcohol use. Tuberculin skin testing (TST), HIV, and interferon-gamma release assay (IGRA) were negative. Esophagogastroduodenoscopy(EGD) showed diffuse ulcerated thickened gastric folds with negative gastric mucosal biopsies. Computed Tomography Abdomen and Pelvis (CT A/P) with contrast revealed multiple enlarged intraabdominal lymph nodes, irregular thickening of the gastric mucosa, and innumerable hypodense splenic lesions(A). Endoscopic Ultrasound (EUS) with fine needle aspiration biopsy (FNAB) of intraabdominal lymph nodes showed scant fibrinopurulent material that was Acid-fast bacteria (AFB) negative. Flow cytometry was unremarkable. Biopsy of axillary lymph nodes showed caseating granulomas(B). The patient was diagnosed with disseminated TB involving the stomach and spleen. Anti-TB therapy led to symptom resolution and weight gain in six months(C).
Discussion: The incidence of TB in Nicaragua (45/100,000) is higher than in the USA, which is (3/100,000). The diagnosis of GI TB mimics other conditions such as inflammatory bowel disease, peptic ulcer disease, or malignancy. Isolated splenic TB can present with jaundice and hepatosplenomegaly. While TST and IGRA are frequently positive in patients with GITB and STB, a negative TST or IGRA does not rule out active TB. The sensitivity for detecting GI TB through AFB with upper EGD with tissue sampling through biopsy or mucosal resection is low. FNAB may reach the deeper submucosa more effectively to locate caseating granulomas/acid-fast bacillus. STB may reveal hypodense splenic lesions on CT A/P. The recommended treatment for GITB and STB is a regimen of anti-TB therapy.
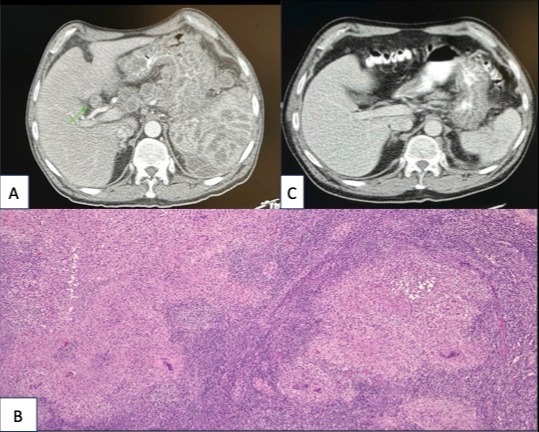
Figure: A: CT abdomen/pelvis with contrast demonstrating multiple enlarged lymph nodes and irregular thickening of the gastric mucosa in the fundus and body. Extensive mesenteric, retroperitoneal lymphadenopathy, mediastinal adenopathy, and nonspecific innumerable hypodense splenic lesions were observed.
B: Biopsy from axillary lymph node showing granulomatous inflammatory changes.
C: CT abdomen/pelvis with contrast after six months of anti-TB therapy showing significant resolution.
B: Biopsy from axillary lymph node showing granulomatous inflammatory changes.
C: CT abdomen/pelvis with contrast after six months of anti-TB therapy showing significant resolution.
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Abirami Rajendiran indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Jonathan Nunez indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
Theja Channapragada, DO, MBA, MS1, Abirami Rajendiran, MD2, Arkady Broder, MD3, Jonathan Nunez, MD4, Srinivas Channapragada, MD5. P1703 - Disseminated Tuberculosis with Gastrointestinal and Splenic Involvement masquerading as Metastatic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
