Sunday Poster Session
Category: Stomach
P1705 - A Rare Case of Primary Gastric Melanoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Samantha Rollins, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Samantha Rollins, DO, Nisha Sanghani, DO, Nishit Patel, MD, Berhanu Geme, MD, Ayaz Matin, MD, Syeda Absar, MD, Hussam Tayel, MD
St. Luke's University Health Network, Bethlehem, PA
Introduction: Malignant melanoma is a cancer that develops from the malignant transformation of melanocytes derived from neural crest cells. Although the majority of melanoma is identified on the skin, it can also develop in other locations where neural crest cells migrate including the gastrointestinal tract where it is referred to as primary mucosal melanoma. Cutaneous melanoma is the fifth most common type of cancer in the US, however, mucosal melanomas are much less common accounting for only 1-3% of all cases. Primary gastric melanoma are exceedingly rare accounting for less than 2% of all primary mucosal melanoma. Here we present a rare case of primary gastric melanoma.
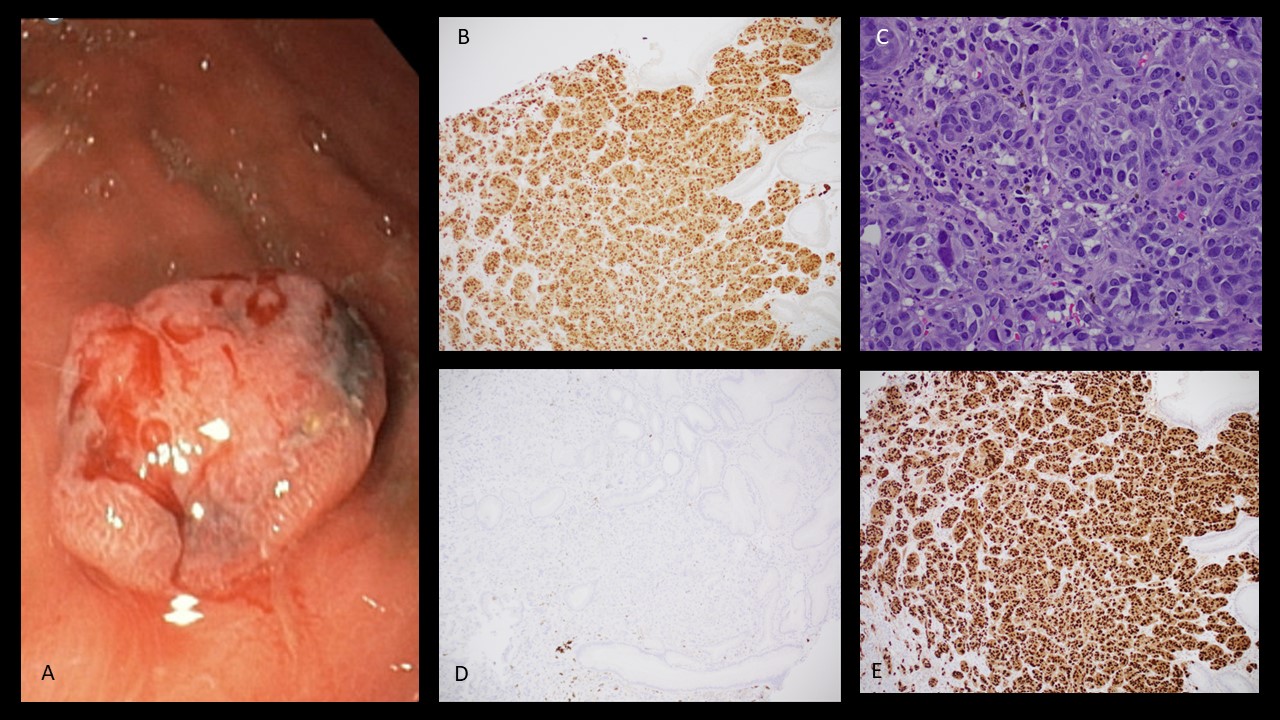
Case Description/Methods: 67-year-old male with a history of atrial fibrillation, DVT, TAVR, diabetes, and prostate cancer status post prostatectomy who presented with progressively worsening postprandial epigastric pain with associated nausea, intermittent melena, and abdominal bloating. Labs on presentation were unremarkable and CT of the abdomen and pelvis demonstrated no acute abnormality. Patient failed to improve with conservative management with PPI therapy and antiemetics and endoscopic evaluation was pursued. EGD was significant for 1.5cm semi-pedunculated, pigmented, ulcerated polyp in the antrum of the stomach that was biopsied with pathology demonstrating malignant epithelioid neoplasm consistent with primary mucosal vs. metastatic melanoma. Subsequently, a comprehensive evaluation of our patient found no primary cutaneous lesion lending to the diagnosis of primary gastric melanoma. Patient has now established with medical oncology and is planned for endoscopic resection with adjuvant immunotherapy.
Discussion: Primary gastric melanoma is an extremely rare malignancy with very few cases reported in literature. Due to the rarity, there are no established diagnostic, staging, or treatment guidelines. Suggested criteria for diagnosis of a primary mucosal lesion includes a biopsy confirmed mucosal lesion without synchronous or prior cutaneous lesion. Surgical resection is recommended for initial intervention with consideration of adjuvant immunotherapy. Early detection is critical as mucosal melanoma is associated with very high mortality. Reported median survival of GI melanoma is approximately 17 months, with median survival of only 5 months in primary gastric melanoma. Poor prognosis is likely related to delayed diagnosis making maintaining clinical suspicion and early recognition paramount for improvement of outcomes.
Disclosures:
Samantha Rollins, DO, Nisha Sanghani, DO, Nishit Patel, MD, Berhanu Geme, MD, Ayaz Matin, MD, Syeda Absar, MD, Hussam Tayel, MD. P1705 - A Rare Case of Primary Gastric Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
St. Luke's University Health Network, Bethlehem, PA
Introduction: Malignant melanoma is a cancer that develops from the malignant transformation of melanocytes derived from neural crest cells. Although the majority of melanoma is identified on the skin, it can also develop in other locations where neural crest cells migrate including the gastrointestinal tract where it is referred to as primary mucosal melanoma. Cutaneous melanoma is the fifth most common type of cancer in the US, however, mucosal melanomas are much less common accounting for only 1-3% of all cases. Primary gastric melanoma are exceedingly rare accounting for less than 2% of all primary mucosal melanoma. Here we present a rare case of primary gastric melanoma.
Case Description/Methods: 67-year-old male with a history of atrial fibrillation, DVT, TAVR, diabetes, and prostate cancer status post prostatectomy who presented with progressively worsening postprandial epigastric pain with associated nausea, intermittent melena, and abdominal bloating. Labs on presentation were unremarkable and CT of the abdomen and pelvis demonstrated no acute abnormality. Patient failed to improve with conservative management with PPI therapy and antiemetics and endoscopic evaluation was pursued. EGD was significant for 1.5cm semi-pedunculated, pigmented, ulcerated polyp in the antrum of the stomach that was biopsied with pathology demonstrating malignant epithelioid neoplasm consistent with primary mucosal vs. metastatic melanoma. Subsequently, a comprehensive evaluation of our patient found no primary cutaneous lesion lending to the diagnosis of primary gastric melanoma. Patient has now established with medical oncology and is planned for endoscopic resection with adjuvant immunotherapy.
Discussion: Primary gastric melanoma is an extremely rare malignancy with very few cases reported in literature. Due to the rarity, there are no established diagnostic, staging, or treatment guidelines. Suggested criteria for diagnosis of a primary mucosal lesion includes a biopsy confirmed mucosal lesion without synchronous or prior cutaneous lesion. Surgical resection is recommended for initial intervention with consideration of adjuvant immunotherapy. Early detection is critical as mucosal melanoma is associated with very high mortality. Reported median survival of GI melanoma is approximately 17 months, with median survival of only 5 months in primary gastric melanoma. Poor prognosis is likely related to delayed diagnosis making maintaining clinical suspicion and early recognition paramount for improvement of outcomes.
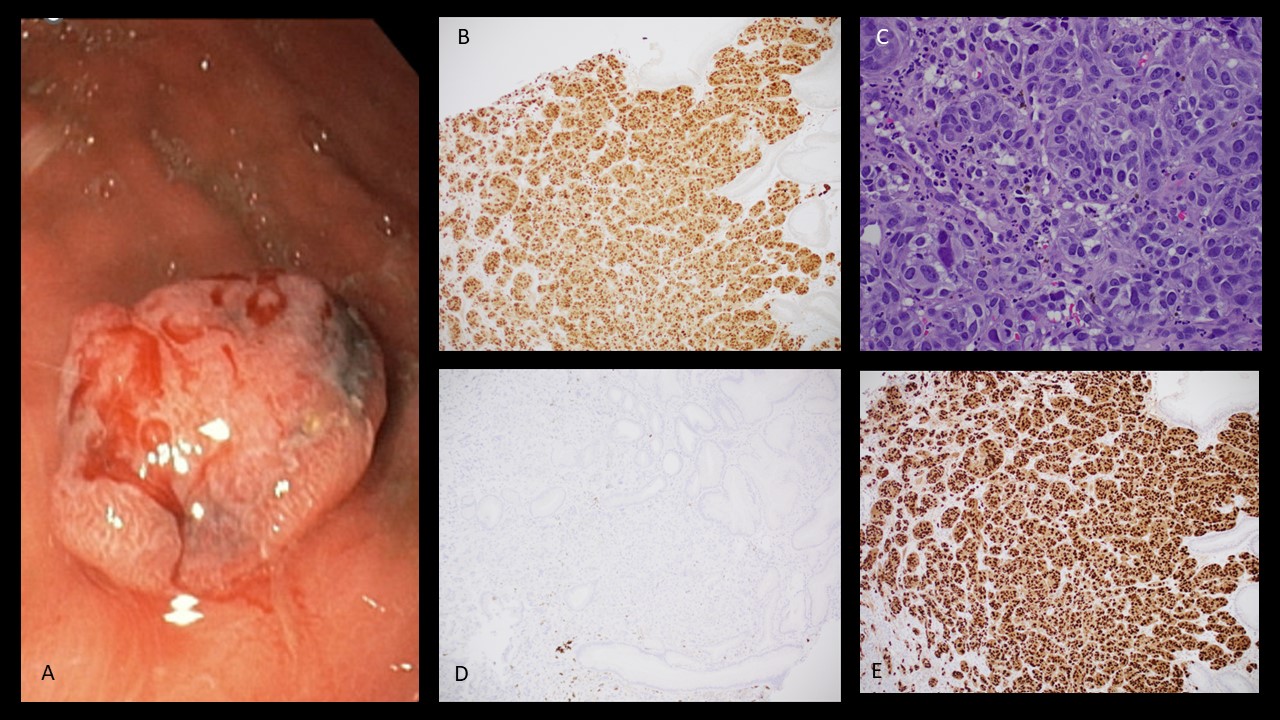
Figure: A. Endoscopic photo of gastric polyp with pathology diagnosing melanoma
B. MITF-1
C. H&E
D. BRAF V600E
E. PRAME
B. MITF-1
C. H&E
D. BRAF V600E
E. PRAME
Disclosures:
Samantha Rollins indicated no relevant financial relationships.
Nisha Sanghani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Ayaz Matin indicated no relevant financial relationships.
Syeda Absar indicated no relevant financial relationships.
Hussam Tayel indicated no relevant financial relationships.
Samantha Rollins, DO, Nisha Sanghani, DO, Nishit Patel, MD, Berhanu Geme, MD, Ayaz Matin, MD, Syeda Absar, MD, Hussam Tayel, MD. P1705 - A Rare Case of Primary Gastric Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
