Monday Poster Session
Category: Biliary/Pancreas
P1711 - Impact of Prior NSAID Use on Clinical Outcomes in Patients Hospitalized With Acute Pancreatitis: A Retrospective Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Mythili Menon Pathiyil, MD
Saint Vincent Hospital
Worcester, MA
Presenting Author(s)
Mythili Menon Pathiyil, MD, Rajaeswaran Chinnamuthu, MD, Rhea Bohra, MD, Priya Pandey, MD, Shreyash Parajuli, MD, Shiksha Joshi, MD, Harinivaas Shanmugavel Geetha, MD, George Abraham, MD, MPH
Saint Vincent Hospital, Worcester, MA
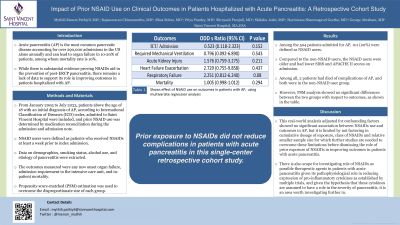
Introduction: Acute pancreatitis (AP) is the most common pancreatic disease accounting for over 290,000 admissions in the US alone annually and can lead to organ failure in 10-20% of patients, among whom mortality rate is 10%. While there is substantial evidence proving NSAIDs aid in the prevention of post-ERCP pancreatitis, there remains a lack of data to support its role in improving outcomes in patients hospitalized with AP.
Methods: From January 2005 to July 2023, patients above the age of 18 with an initial diagnosis of AP, according to International Classification of Diseases (ICD) codes, admitted to Saint Vincent Hospital were included, and prior NSAID use was determined by medication reconciliation during the admission and admission note.
NSAID users were defined as patients who received NSAIDs at least a week prior to index admission. Data on demographics, smoking status, alcohol use, and etiology of pancreatitis were extracted. The outcomes measured were any new onset organ failure, length of hospital stay, admission requirement to the intensive care unit, and in-patient mortality. Propensity score-matched (PSM) estimation was used to overcome the disproportionate size of each group.
Results: Among the 504 patients admitted for AP, 101 (20%) were defined as NSAID users. Compared to the non-NSAID users, the NSAID users were older and had lower SIRS and APACHE II scores on admission. Among all, 2 patients had died of complications of AP, and both were in the non-NSAID user group. However, PSM analysis showed no significant differences between the two groups with respect to outcomes, as shown in the table.
Discussion: This real-world analysis with adjustment for confounding factors showed no significant association between NSAIDs use and outcomes in AP, but it is limited by not factoring in cumulative dosage of exposure, class of NSAIDs and relative smaller sample size for which further studies are needed to overcome these limitations before dismissing the role of prior exposure of NSAIDs in improving outcomes in patients with acute pancreatitis. There is also scope for investigating role of NSAIDs as possible therapeutic agents in patients with acute pancreatitis given its pathophysiological role in reducing expression of pro-inflammatory cytokines as established by multiple trials, and given the hypothesis that these cytokines are assumed to have a role in the severity of pancreatitis, it is an area worth investigating further in.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mythili Menon Pathiyil, MD, Rajaeswaran Chinnamuthu, MD, Rhea Bohra, MD, Priya Pandey, MD, Shreyash Parajuli, MD, Shiksha Joshi, MD, Harinivaas Shanmugavel Geetha, MD, George Abraham, MD, MPH. P1711 - Impact of Prior NSAID Use on Clinical Outcomes in Patients Hospitalized With Acute Pancreatitis: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Saint Vincent Hospital, Worcester, MA
Introduction: Acute pancreatitis (AP) is the most common pancreatic disease accounting for over 290,000 admissions in the US alone annually and can lead to organ failure in 10-20% of patients, among whom mortality rate is 10%. While there is substantial evidence proving NSAIDs aid in the prevention of post-ERCP pancreatitis, there remains a lack of data to support its role in improving outcomes in patients hospitalized with AP.
Methods: From January 2005 to July 2023, patients above the age of 18 with an initial diagnosis of AP, according to International Classification of Diseases (ICD) codes, admitted to Saint Vincent Hospital were included, and prior NSAID use was determined by medication reconciliation during the admission and admission note.
NSAID users were defined as patients who received NSAIDs at least a week prior to index admission. Data on demographics, smoking status, alcohol use, and etiology of pancreatitis were extracted. The outcomes measured were any new onset organ failure, length of hospital stay, admission requirement to the intensive care unit, and in-patient mortality. Propensity score-matched (PSM) estimation was used to overcome the disproportionate size of each group.
Results: Among the 504 patients admitted for AP, 101 (20%) were defined as NSAID users. Compared to the non-NSAID users, the NSAID users were older and had lower SIRS and APACHE II scores on admission. Among all, 2 patients had died of complications of AP, and both were in the non-NSAID user group. However, PSM analysis showed no significant differences between the two groups with respect to outcomes, as shown in the table.
Discussion: This real-world analysis with adjustment for confounding factors showed no significant association between NSAIDs use and outcomes in AP, but it is limited by not factoring in cumulative dosage of exposure, class of NSAIDs and relative smaller sample size for which further studies are needed to overcome these limitations before dismissing the role of prior exposure of NSAIDs in improving outcomes in patients with acute pancreatitis. There is also scope for investigating role of NSAIDs as possible therapeutic agents in patients with acute pancreatitis given its pathophysiological role in reducing expression of pro-inflammatory cytokines as established by multiple trials, and given the hypothesis that these cytokines are assumed to have a role in the severity of pancreatitis, it is an area worth investigating further in.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mythili Menon Pathiyil indicated no relevant financial relationships.
Rajaeswaran Chinnamuthu indicated no relevant financial relationships.
Rhea Bohra indicated no relevant financial relationships.
Priya Pandey indicated no relevant financial relationships.
Shreyash Parajuli indicated no relevant financial relationships.
Shiksha Joshi indicated no relevant financial relationships.
Harinivaas Shanmugavel Geetha indicated no relevant financial relationships.
George Abraham indicated no relevant financial relationships.
Mythili Menon Pathiyil, MD, Rajaeswaran Chinnamuthu, MD, Rhea Bohra, MD, Priya Pandey, MD, Shreyash Parajuli, MD, Shiksha Joshi, MD, Harinivaas Shanmugavel Geetha, MD, George Abraham, MD, MPH. P1711 - Impact of Prior NSAID Use on Clinical Outcomes in Patients Hospitalized With Acute Pancreatitis: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
