Sunday Poster Session
Category: Stomach
P1614 - Unveiling the Hidden Toll: Disparities in Gastric Ulcer Related Mortality – Insights from a CDC WONDER Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Fariha Hasan, MD
Cooper University Hospital
Philadelphia, PA
Presenting Author(s)
Fariha Hasan, MD1, Fawad Ahmed, MBBS2, Jawad Ahmed, MBBS2, Saman Afzal, MBBS2, Nimra Afzal, MBBS2, Muhammad Ammar Ur Rahman, MBBS2, Muhammad Shahzil, MD3, Luqman Munir, MBBS2, Amna Khalid, MBBS2
1Cooper University Hospital, Philadelphia, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA
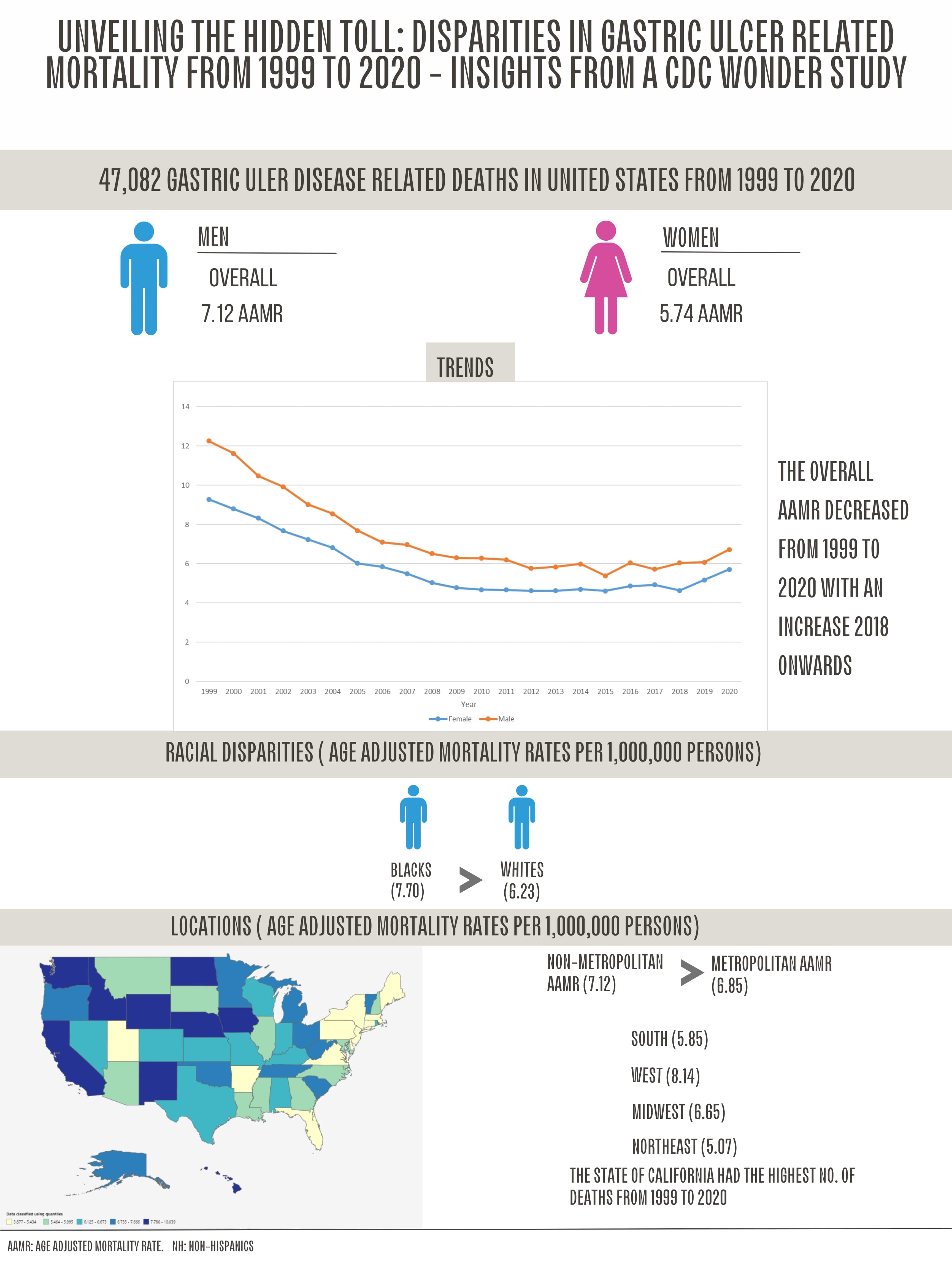
Introduction: Gastric ulcers, a form of peptic ulcer disease (PUD), are open sores on the stomach's inner lining caused by stomach acid and digestive enzymes. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports an annual incidence of 0.1% to 0.3% and a prevalence of about 1%. This study aims to analyze mortality trends related to gastric ulcer disease from 1999 to 2020, focusing on age-adjusted mortality rates to identify disparities across different age groups, races, ethnicities, urban and suburban areas, and census regions.
Methods: We analyzed Death Certificates from the Centers for Disease Control and Prevention (CDC) Wide-Ranging Online Data for Epidemiological Research (WONDER) database from 1999-2020. AAMR per 1,000,000 people and annual percent change (APC) with a 95% confidence interval were determined. We then used the Joinpoint Regression Program to obtain trends amongst epidemiological (race, ethnicity, gender, age) and demographic (census region, 2013 urbanization status) groups.
Results: From 1999 to 2009, age-adjusted mortality rates (AAMRs) due to gastric ulcer disease significantly decreased with an annual percent change (APC) of -6.68%. This trend plateaued from 2009 to 2018 (APC -0.19%) but rose sharply from 2019 to 2020 (APC 8.47%). The majority of deaths occurred in medical inpatient facilities and at home, both of which saw dramatic increases after 2018, with APCs of 10.06% and 16.73%, respectively. A comparative analysis of males and females revealed a significant rise in mortality rates post-2018, with APCs of 3.11% and 9.73%, respectively. The Midwest had the highest mortality rates despite a decreasing trend from 1999 to 2010 (APC -6.41%). However, all regions, including the Midwest, have experienced rising mortality rates in recent years. Mortality rates among Whites were comparable to those among African Americans/Blacks and other
ethnicities, including Hispanics/Latinos, up to 2018. After 2018, mortality rates increased for these groups, with APCs of 7.25%, 2.39%, and 7.97%, respectively. Urban areas saw a higher change in mortality trends (APC 11.87%) compared to suburban/micropolitan areas (APC 2.23%) from 2018 to 2020.
Discussion: Since 2018, mortality rates related to gastric ulcers have been on the rise in the US. Persistent demographic and geographic disparities, particularly the gap between urban and suburban areas, highlight the urgent need for further investigation and targeted interventions to improve outcomes across all groups.
Disclosures:
Fariha Hasan, MD1, Fawad Ahmed, MBBS2, Jawad Ahmed, MBBS2, Saman Afzal, MBBS2, Nimra Afzal, MBBS2, Muhammad Ammar Ur Rahman, MBBS2, Muhammad Shahzil, MD3, Luqman Munir, MBBS2, Amna Khalid, MBBS2. P1614 - Unveiling the Hidden Toll: Disparities in Gastric Ulcer Related Mortality – Insights from a CDC WONDER Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Philadelphia, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Gastric ulcers, a form of peptic ulcer disease (PUD), are open sores on the stomach's inner lining caused by stomach acid and digestive enzymes. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports an annual incidence of 0.1% to 0.3% and a prevalence of about 1%. This study aims to analyze mortality trends related to gastric ulcer disease from 1999 to 2020, focusing on age-adjusted mortality rates to identify disparities across different age groups, races, ethnicities, urban and suburban areas, and census regions.
Methods: We analyzed Death Certificates from the Centers for Disease Control and Prevention (CDC) Wide-Ranging Online Data for Epidemiological Research (WONDER) database from 1999-2020. AAMR per 1,000,000 people and annual percent change (APC) with a 95% confidence interval were determined. We then used the Joinpoint Regression Program to obtain trends amongst epidemiological (race, ethnicity, gender, age) and demographic (census region, 2013 urbanization status) groups.
Results: From 1999 to 2009, age-adjusted mortality rates (AAMRs) due to gastric ulcer disease significantly decreased with an annual percent change (APC) of -6.68%. This trend plateaued from 2009 to 2018 (APC -0.19%) but rose sharply from 2019 to 2020 (APC 8.47%). The majority of deaths occurred in medical inpatient facilities and at home, both of which saw dramatic increases after 2018, with APCs of 10.06% and 16.73%, respectively. A comparative analysis of males and females revealed a significant rise in mortality rates post-2018, with APCs of 3.11% and 9.73%, respectively. The Midwest had the highest mortality rates despite a decreasing trend from 1999 to 2010 (APC -6.41%). However, all regions, including the Midwest, have experienced rising mortality rates in recent years. Mortality rates among Whites were comparable to those among African Americans/Blacks and other
ethnicities, including Hispanics/Latinos, up to 2018. After 2018, mortality rates increased for these groups, with APCs of 7.25%, 2.39%, and 7.97%, respectively. Urban areas saw a higher change in mortality trends (APC 11.87%) compared to suburban/micropolitan areas (APC 2.23%) from 2018 to 2020.
Discussion: Since 2018, mortality rates related to gastric ulcers have been on the rise in the US. Persistent demographic and geographic disparities, particularly the gap between urban and suburban areas, highlight the urgent need for further investigation and targeted interventions to improve outcomes across all groups.
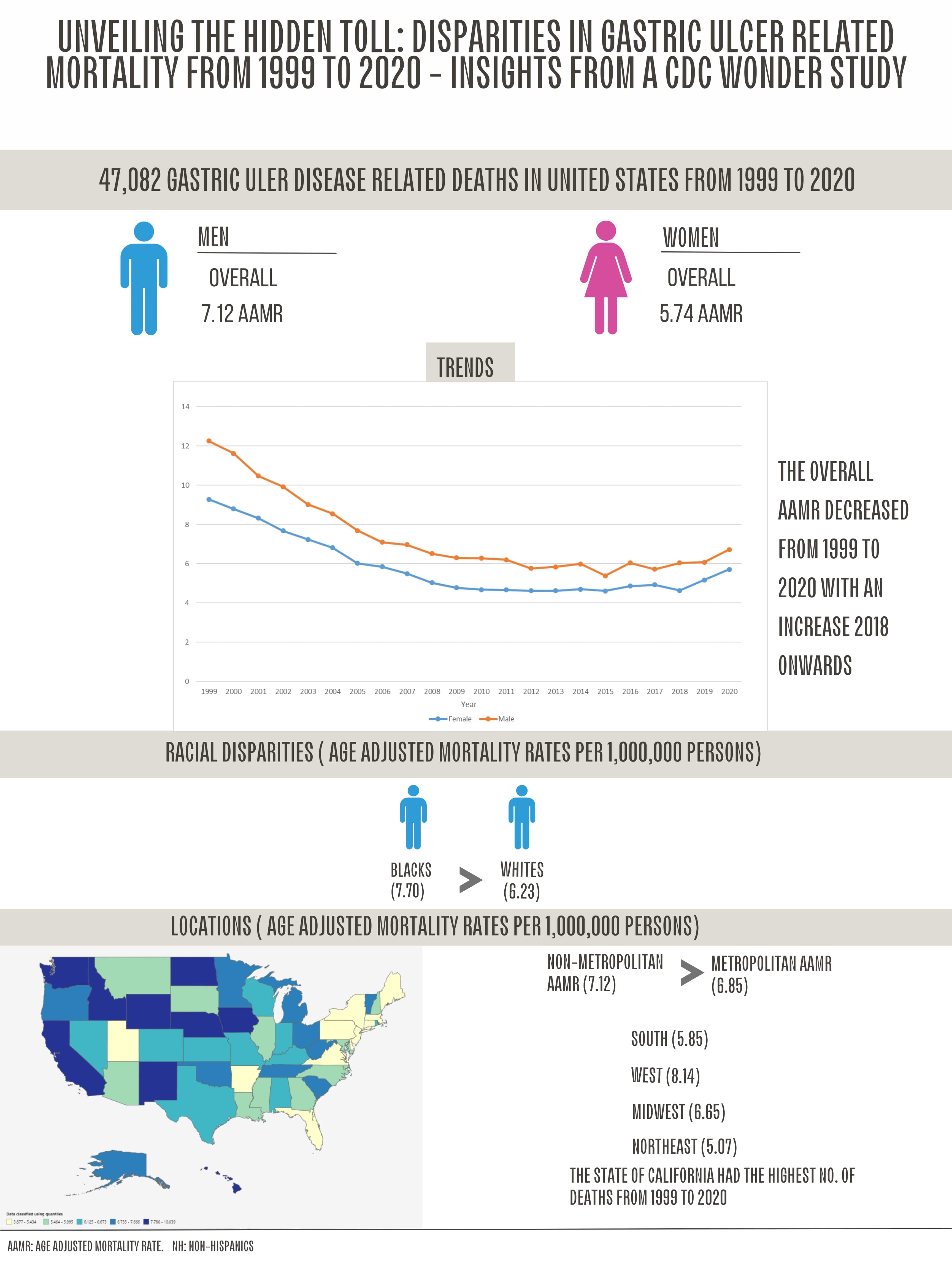
Figure: Disparities in Gastric Ulcer Related Mortality from 1999 to 2020
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Fawad Ahmed indicated no relevant financial relationships.
Jawad Ahmed indicated no relevant financial relationships.
Saman Afzal indicated no relevant financial relationships.
Nimra Afzal indicated no relevant financial relationships.
Muhammad Ammar Ur Rahman indicated no relevant financial relationships.
Muhammad Shahzil indicated no relevant financial relationships.
Luqman Munir indicated no relevant financial relationships.
Amna Khalid indicated no relevant financial relationships.
Fariha Hasan, MD1, Fawad Ahmed, MBBS2, Jawad Ahmed, MBBS2, Saman Afzal, MBBS2, Nimra Afzal, MBBS2, Muhammad Ammar Ur Rahman, MBBS2, Muhammad Shahzil, MD3, Luqman Munir, MBBS2, Amna Khalid, MBBS2. P1614 - Unveiling the Hidden Toll: Disparities in Gastric Ulcer Related Mortality – Insights from a CDC WONDER Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
