Sunday Poster Session
Category: Stomach
P1628 - Fundic Gland Polyposis With Chronic PPI Use: Is Surveillance Warranted?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- LL
Lauren Lally, MD
Robert Wood Johnson University Hospital
New Brunswick, NJ
Presenting Author(s)
Lauren Lally, MD1, Anish V. Patel, MD2, Isago Jerrett, MD2
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: In Western countries where the prevalence of proton pump inhibitor (PPI) is more common, gastric polyps encountered are commonly fundic gland polyps (FGP). These polyps are typically benign and do not require surveillance. We introduce a case of a patient with FGPs demonstrating dysplasia.
Case Description/Methods: An 87 y/o Caucasian male with gastroesophageal reflux disease (GERD) and benign prostatic hyperplasia presented to the clinic for chronic GERD. He had been on omeprazole 40 mg daily for over 30 years. Reported biweekly symptoms without any associated food triggers. Given the patient’s age, gender and ethnicity, decision was made to undergo endoscopy for Barrett’s esophagus screening.
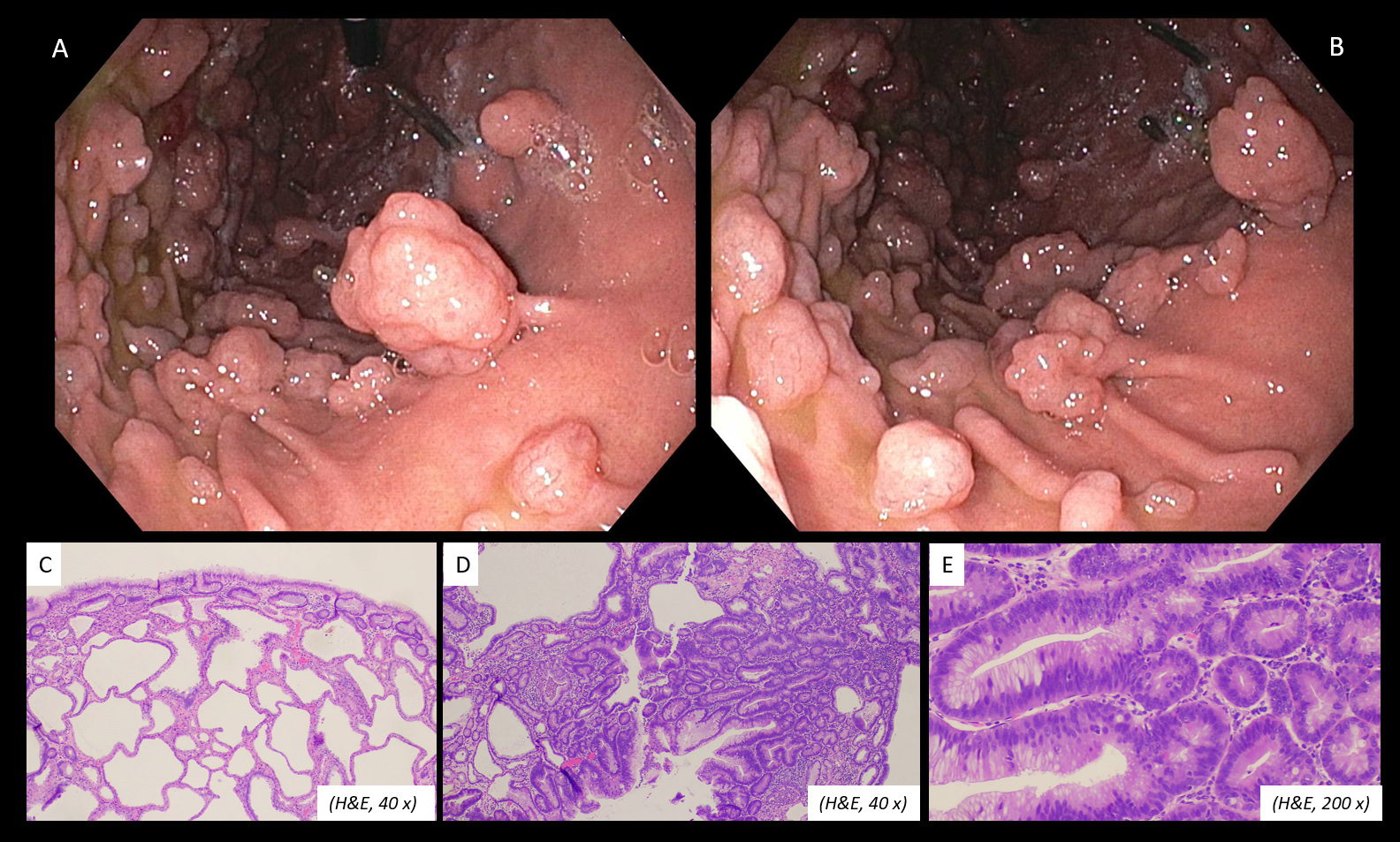
Endoscopy revealed sheets of FGPs, the largest measuring 1.8 cm. The largest ten polyps were resected with pathology showing benign FGPs. There was no evidence of Barrett’s esophagus. He did not want to discontinue or taper PPI therapy given severe GERD in the past during attempts at dose reduction or discontinuation. He does not have a family history of familial adenomatous polyposis (FAP), and had routine screening colonoscopies identifying only 1-2 sub-centimeter tubular adenomas. He then underwent repeat endoscopy one year later for surveillance of his gastric polyps. Endoscopy again revealed sheets of FGPs. Fifteen of the largest FGPs were resected with hot snare. The total aggregate of combined polyps measured 4.7 x 4.5 x 1.2 cm and pathology this time demonstrated FGPs with focal low-grade dysplasia. The decision was made to do surveillance endoscopy every 6 months for further evaluation.
Discussion: FGPs rarely show dysplasia, and thus there is no recommendation for surveillance endoscopy. When fundic gland polyposis is detected, a family history of polyposis and history of PPI use should be sought. In our patient who had no dysplasia in his largest polyps on initial endoscopy, but one year later showed FGPs with low grade dysplasia begs the question, should we be doing surveillance endoscopy? In the absence of FAP, our patient’s gastric polyposis was attributed to chronic PPI use. This is a unique case given the sheer number of FGPs identified endoscopically, however should there be guidelines on the number of polyps identified to warrant repeat endoscopy? PPI discontinuation should be considered, and it may be reasonable to perform surveillance endoscopy every 6-12 months in such cases of striking fundic gland polyposis.
Disclosures:
Lauren Lally, MD1, Anish V. Patel, MD2, Isago Jerrett, MD2. P1628 - Fundic Gland Polyposis With Chronic PPI Use: Is Surveillance Warranted?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: In Western countries where the prevalence of proton pump inhibitor (PPI) is more common, gastric polyps encountered are commonly fundic gland polyps (FGP). These polyps are typically benign and do not require surveillance. We introduce a case of a patient with FGPs demonstrating dysplasia.
Case Description/Methods: An 87 y/o Caucasian male with gastroesophageal reflux disease (GERD) and benign prostatic hyperplasia presented to the clinic for chronic GERD. He had been on omeprazole 40 mg daily for over 30 years. Reported biweekly symptoms without any associated food triggers. Given the patient’s age, gender and ethnicity, decision was made to undergo endoscopy for Barrett’s esophagus screening.
Endoscopy revealed sheets of FGPs, the largest measuring 1.8 cm. The largest ten polyps were resected with pathology showing benign FGPs. There was no evidence of Barrett’s esophagus. He did not want to discontinue or taper PPI therapy given severe GERD in the past during attempts at dose reduction or discontinuation. He does not have a family history of familial adenomatous polyposis (FAP), and had routine screening colonoscopies identifying only 1-2 sub-centimeter tubular adenomas. He then underwent repeat endoscopy one year later for surveillance of his gastric polyps. Endoscopy again revealed sheets of FGPs. Fifteen of the largest FGPs were resected with hot snare. The total aggregate of combined polyps measured 4.7 x 4.5 x 1.2 cm and pathology this time demonstrated FGPs with focal low-grade dysplasia. The decision was made to do surveillance endoscopy every 6 months for further evaluation.
Discussion: FGPs rarely show dysplasia, and thus there is no recommendation for surveillance endoscopy. When fundic gland polyposis is detected, a family history of polyposis and history of PPI use should be sought. In our patient who had no dysplasia in his largest polyps on initial endoscopy, but one year later showed FGPs with low grade dysplasia begs the question, should we be doing surveillance endoscopy? In the absence of FAP, our patient’s gastric polyposis was attributed to chronic PPI use. This is a unique case given the sheer number of FGPs identified endoscopically, however should there be guidelines on the number of polyps identified to warrant repeat endoscopy? PPI discontinuation should be considered, and it may be reasonable to perform surveillance endoscopy every 6-12 months in such cases of striking fundic gland polyposis.
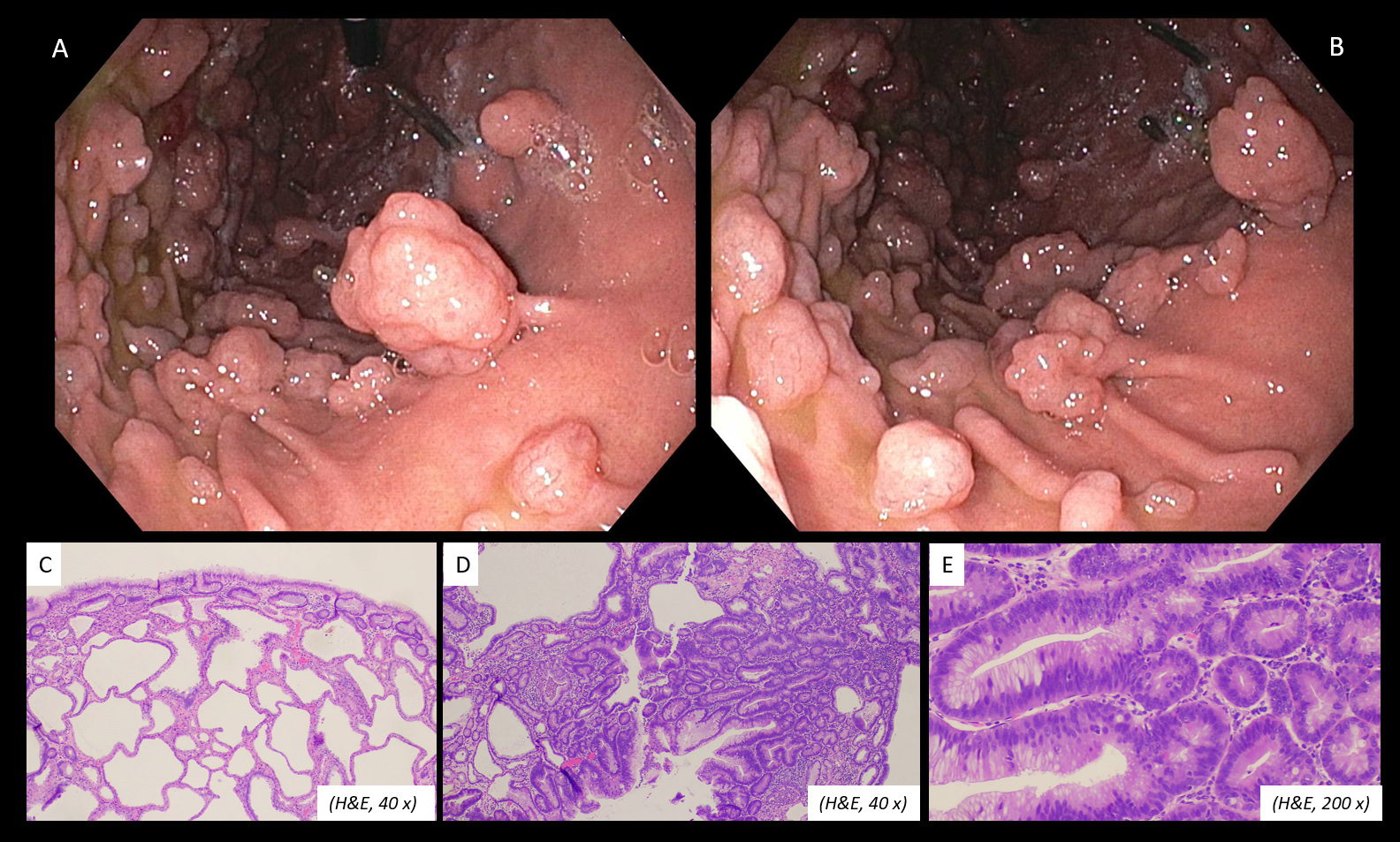
Figure: Figure 1: Fundic gland polys (A & B), fundic gland polyps without dysplasia (C), in contrast to an area of the polyp demonstrating focal low-grade dysplasia (D & E)
Disclosures:
Lauren Lally indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Isago Jerrett indicated no relevant financial relationships.
Lauren Lally, MD1, Anish V. Patel, MD2, Isago Jerrett, MD2. P1628 - Fundic Gland Polyposis With Chronic PPI Use: Is Surveillance Warranted?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
