Sunday Poster Session
Category: Stomach
P1630 - Rare Collagenous Gastritis Presenting as Epigastric Pain in Teenage Female
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brandon T. Wiggins, DO, MPH
Ascension Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Grand Blanc, MI
Introduction: Collagenous gastritis (CG) is a rare condition with an estimated prevalence of 13 cases per every 100,000 EGDs, with a bimodal distribution of 10-19 and >60 years of age. We present the case of a young female with prolonged, nonspecific abdominal complaints of nausea and epigastric pain who, after further investigation, was found to have CG.
Case Description/Methods: 18 year old female presented with epigastric pain and postprandial nausea for one year. She denied any GI bleeding, diarrhea, constipation or weight loss. She attempted acid reducing medications with no benefit. She admitted to rare NSAID use and denied any food allergies nor family history of GI malignancy.
She had a H. pylori breath test that was negative before endoscopy.
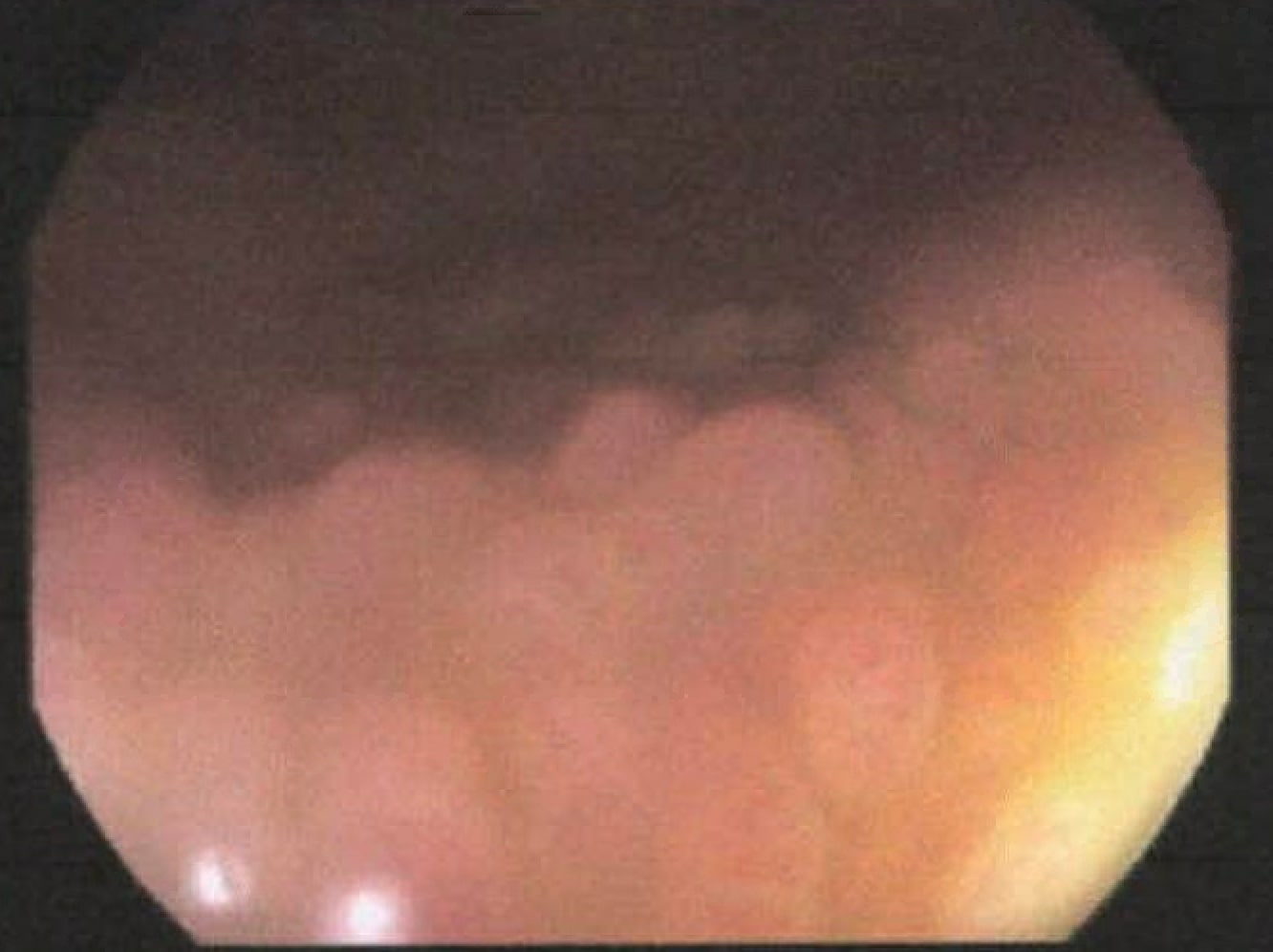
EGD demonstrated atrophic changes in the gastric body and fundus suspicious for H. pylori infectious or MALT lymphoma. Biopsies were negative for celiac sprue and positive for H. pylori gastritis but lymphoid infiltrate was dense, concerning for MALT lymphoma and were sent to a tertiary facility. Biopsies were re-examined and determined not to be related to H. pylori nor MALT lymphoma but dense collagen deposits consistent with CG. She was started on twice daily proton pump inhibitor with improvement in symptoms.
Discussion: Clinical manifestations of CG can be nonspecific including abdominal pain, weight loss, nausea, diarrhea and anemia. In pediatric patients inflammation is limited to the body of the stomach, while adults display mostly an antral predominance. Although the exact etiology is unclear, theories suggest associations with inflammation from autoimmune disease, medications, and infections like H. pylori. Pathohistological diagnosis includes variable deposition of inflammatory infiltrates in the lamina propria and thick collagen in the subepithelium of 10 µm thickness. Chronic inflammation causes atrophic changes in mucosal glands leading to a depressed appearance between nodular lesions visible on endoscopy. Due to its infrequent occurrence, treatment including PPIs, steroids, mesalamine, and diet alteration have been tried with varying success, and there is currently no standardized therapy.
Although rare, gastroenterologists should be aware of CG and recognize the endoscopic appearance. Additional case reports and research will help further clinician’s awareness of clinical presentation, endoscopic and pathohistological appearance and treatment.
Disclosures:
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2. P1630 - Rare Collagenous Gastritis Presenting as Epigastric Pain in Teenage Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Grand Blanc, MI
Introduction: Collagenous gastritis (CG) is a rare condition with an estimated prevalence of 13 cases per every 100,000 EGDs, with a bimodal distribution of 10-19 and >60 years of age. We present the case of a young female with prolonged, nonspecific abdominal complaints of nausea and epigastric pain who, after further investigation, was found to have CG.
Case Description/Methods: 18 year old female presented with epigastric pain and postprandial nausea for one year. She denied any GI bleeding, diarrhea, constipation or weight loss. She attempted acid reducing medications with no benefit. She admitted to rare NSAID use and denied any food allergies nor family history of GI malignancy.
She had a H. pylori breath test that was negative before endoscopy.
EGD demonstrated atrophic changes in the gastric body and fundus suspicious for H. pylori infectious or MALT lymphoma. Biopsies were negative for celiac sprue and positive for H. pylori gastritis but lymphoid infiltrate was dense, concerning for MALT lymphoma and were sent to a tertiary facility. Biopsies were re-examined and determined not to be related to H. pylori nor MALT lymphoma but dense collagen deposits consistent with CG. She was started on twice daily proton pump inhibitor with improvement in symptoms.
Discussion: Clinical manifestations of CG can be nonspecific including abdominal pain, weight loss, nausea, diarrhea and anemia. In pediatric patients inflammation is limited to the body of the stomach, while adults display mostly an antral predominance. Although the exact etiology is unclear, theories suggest associations with inflammation from autoimmune disease, medications, and infections like H. pylori. Pathohistological diagnosis includes variable deposition of inflammatory infiltrates in the lamina propria and thick collagen in the subepithelium of 10 µm thickness. Chronic inflammation causes atrophic changes in mucosal glands leading to a depressed appearance between nodular lesions visible on endoscopy. Due to its infrequent occurrence, treatment including PPIs, steroids, mesalamine, and diet alteration have been tried with varying success, and there is currently no standardized therapy.
Although rare, gastroenterologists should be aware of CG and recognize the endoscopic appearance. Additional case reports and research will help further clinician’s awareness of clinical presentation, endoscopic and pathohistological appearance and treatment.
Figure: Endoscopic Image Demonstrating Atrophic Gastritis mixed with Areas of Nodularity Consistent with Collagenous Gastritis
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
Se Yeon Kim indicated no relevant financial relationships.
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2. P1630 - Rare Collagenous Gastritis Presenting as Epigastric Pain in Teenage Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

