Sunday Poster Session
Category: Stomach
P1631 - Perforated Gastric Remnant Ulcer in Roux-en-Y Gastric Bypass Patient During Esophagogastroduodenoscopy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brandon T. Wiggins, DO, MPH
Ascension Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2, Jake Burch, DO3, Justin Miller, DO4, Derek Thigpin, DO5
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Grand Blanc, MI; 3Ascension Genesys, Swartz Creek, MI; 4Ascension Genesys Hospital, Clarkston, MI; 5Flint Gastroenterology Associates, Milford, MI
Introduction: Roux-en-Y gastric bypass (RYGB) creates a gastric pouch by separating it from the distal stomach and proximal small intestine, which restricts food consumption. Although RYGB aids in weight reduction and obesity co-morbidities, it is linked with complications like malabsorption and nephrolithiasis, and rarely gastric remnant ulcer (GRU). Given the altered anatomy in RYGB, GRU is difficult to visualize using traditional endoscopy, making diagnosis difficult. Early detection and treatment of GRU are essential to avoid complications, such as GRU perforation, which is a surgical emergency.
Case Description/Methods: 60 year old female with RYGB presented for epigastric pain. Her pain had occurred abruptly 24 hours before presentation and was severe, constant and non-radiating. She admitted to using ibuprofen daily for 2 months.
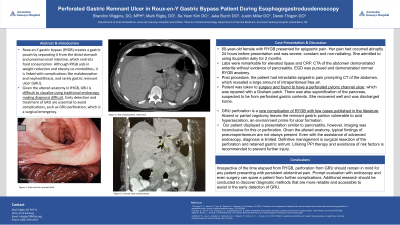
Labs were remarkable for elevated lipase and CRP. CTA of the abdomen demonstrated enteritis without evidence of pancreatitis. EGD was pursued and demonstrated normal RYGB anatomy. Post procedure, the patient had intractable epigastric pain prompting CT of the abdomen, which revealed a large amount of intraperitoneal free air.
Patient was taken to surgery and found to have a perforated pyloric channel ulcer, which was repaired with a Graham patch. There was also saponification of the pancreas, suspected to be from perforated gastric contents. She recovered well and was discharged home.
Discussion: GRU perforation is a rare complication of RYGB with few cases published in the literature. Absent or partial vagotomy leaves the remnant gastric portion vulnerable to acid hypersecretion, an environment prime for ulcer formation.
Our patient displayed a presentation similar to pancreatitis, however, imaging was inconclusive for this or perforation. Given the altered anatomy, typical findings of pneumoperitoneum are not always present. Even with the assistance of advanced endoscopy, diagnosis is limited. Definitive management is surgical resection of the perforation and retained gastric antrum. Lifelong PPI therapy and avoidance of risk factors is recommended to prevent further injury.
Irrespective of the time elapsed from RYGB, perforation from GRU should remain in mind for any patient presenting with persistent abdominal pain. Prompt evaluation with endoscopy and even surgery can spare a patient from further complications. Additional research should be conducted in order to discover diagnostic methods that are more reliable and accessible to assist in the early detection of GRU.

Disclosures:
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2, Jake Burch, DO3, Justin Miller, DO4, Derek Thigpin, DO5. P1631 - Perforated Gastric Remnant Ulcer in Roux-en-Y Gastric Bypass Patient During Esophagogastroduodenoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Grand Blanc, MI; 3Ascension Genesys, Swartz Creek, MI; 4Ascension Genesys Hospital, Clarkston, MI; 5Flint Gastroenterology Associates, Milford, MI
Introduction: Roux-en-Y gastric bypass (RYGB) creates a gastric pouch by separating it from the distal stomach and proximal small intestine, which restricts food consumption. Although RYGB aids in weight reduction and obesity co-morbidities, it is linked with complications like malabsorption and nephrolithiasis, and rarely gastric remnant ulcer (GRU). Given the altered anatomy in RYGB, GRU is difficult to visualize using traditional endoscopy, making diagnosis difficult. Early detection and treatment of GRU are essential to avoid complications, such as GRU perforation, which is a surgical emergency.
Case Description/Methods: 60 year old female with RYGB presented for epigastric pain. Her pain had occurred abruptly 24 hours before presentation and was severe, constant and non-radiating. She admitted to using ibuprofen daily for 2 months.
Labs were remarkable for elevated lipase and CRP. CTA of the abdomen demonstrated enteritis without evidence of pancreatitis. EGD was pursued and demonstrated normal RYGB anatomy. Post procedure, the patient had intractable epigastric pain prompting CT of the abdomen, which revealed a large amount of intraperitoneal free air.
Patient was taken to surgery and found to have a perforated pyloric channel ulcer, which was repaired with a Graham patch. There was also saponification of the pancreas, suspected to be from perforated gastric contents. She recovered well and was discharged home.
Discussion: GRU perforation is a rare complication of RYGB with few cases published in the literature. Absent or partial vagotomy leaves the remnant gastric portion vulnerable to acid hypersecretion, an environment prime for ulcer formation.
Our patient displayed a presentation similar to pancreatitis, however, imaging was inconclusive for this or perforation. Given the altered anatomy, typical findings of pneumoperitoneum are not always present. Even with the assistance of advanced endoscopy, diagnosis is limited. Definitive management is surgical resection of the perforation and retained gastric antrum. Lifelong PPI therapy and avoidance of risk factors is recommended to prevent further injury.
Irrespective of the time elapsed from RYGB, perforation from GRU should remain in mind for any patient presenting with persistent abdominal pain. Prompt evaluation with endoscopy and even surgery can spare a patient from further complications. Additional research should be conducted in order to discover diagnostic methods that are more reliable and accessible to assist in the early detection of GRU.

Figure: Coronal View Computed Tomography Demonstrating Intraperitoneal Free Air After Esophagogastroduodenoscopy
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
Se Yeon Kim indicated no relevant financial relationships.
Jake Burch indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Derek Thigpin indicated no relevant financial relationships.
Brandon T. Wiggins, DO, MPH1, Mark Rigby, DO2, Se Yeon Kim, DO2, Jake Burch, DO3, Justin Miller, DO4, Derek Thigpin, DO5. P1631 - Perforated Gastric Remnant Ulcer in Roux-en-Y Gastric Bypass Patient During Esophagogastroduodenoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
