Sunday Poster Session
Category: Small Intestine
P1537 - Lupus Enteritis: An Uncommon Presentation of Lupus Diagnosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- VC
Victoria A. Caruso, DO
University of Massachusetts Chan Medical School - Baystate Medical Center
Windsor, CT
Presenting Author(s)
Victoria A. Caruso, DO1, Muhammad Khan, MD2, Kevin Groudan, MD3, Nha Duong, DO2
1University of Massachusetts Chan Medical School - Baystate Medical Center, Windsor, CT; 2University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA
Introduction: Lupus enterocolitis is a rare manifestation of systemic lupus erythematosus (SLE). Diagnosing this condition is challenging without other symptoms specific to SLE as the symptoms overlap with other common abdominal pathologies. We present a case of lupus enteritis as the initial manifestation of SLE.
Case Description/Methods: A 47-year-old African-American female with a medical history of asthma presented to the hospital with three weeks of abdominal pain, nausea and dry heaving. She reported months of joint pain and unintentional weight loss of over 10 pounds within one month. Her bowel movements were normal without diarrhea or bleeding. Family history revealed an aunt with rheumatoid arthritis. Vital signs were normal and labs were notable for a white count of 2.9 k/mm3 and a hemoglobin of 9.3 gm/dL. Computed tomography angiogram (CTA) of the abdomen and pelvis demonstrated normal vasculature and thickening of the small bowel, cecum and ascending colon consistent with enterocolitis. Esophagogastroduodenoscopy and colonoscopy showed normal mucosa without inflammation and normal colonic biopsies. Autoimmune labs were sent for concern for lupus enteritis and revealed low complement C3 (45 mg/dl) and C4 (3 mg/dl). Antinuclear antibody was > 1:1280, anti-smith antibodies > 8.0 and anti-ribonucleic acid antibodies were elevated at 7.3. These findings were consistent with lupus enterocolitis and after discussion with rheumatology, she was started on intravenous (IV) pulse steroids for three days followed by an oral prednisone regimen with marked improvement in her symptoms. She was discharged on prednisone and hydroxychloroquine with rheumatology follow-up.
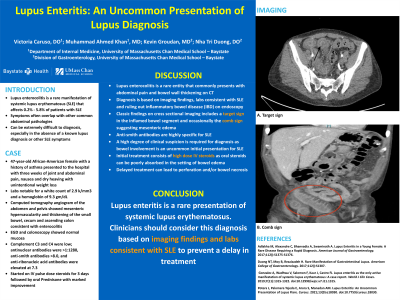
Discussion: Lupus enterocolitis is a rare entity that commonly presents with abdominal pain and bowel wall thickening on CT. Diagnosis is usually made based on imaging findings, labs consistent with SLE and ruling out inflammatory bowel disease (IBD) on endoscopy. The classic findings on cross sectional imaging includes a target sign in the inflamed bowel segment and occasionally the comb sign suggesting mesenteric edema. Anti-smith antibodies are highly specific for SLE. A high degree of clinical suspicion is required for diagnosis as bowel involvement is an uncommon initial presentation for SLE. In our patient, the suspicion stemmed from the appearance of her small bowel on CT, rheumatologic symptoms and lack of IBD. Initial treatment consists of high dose IV steroids as oral steroids can be poorly absorbed in the setting of bowel edema.

Disclosures:
Victoria A. Caruso, DO1, Muhammad Khan, MD2, Kevin Groudan, MD3, Nha Duong, DO2. P1537 - Lupus Enteritis: An Uncommon Presentation of Lupus Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Medical Center, Windsor, CT; 2University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA
Introduction: Lupus enterocolitis is a rare manifestation of systemic lupus erythematosus (SLE). Diagnosing this condition is challenging without other symptoms specific to SLE as the symptoms overlap with other common abdominal pathologies. We present a case of lupus enteritis as the initial manifestation of SLE.
Case Description/Methods: A 47-year-old African-American female with a medical history of asthma presented to the hospital with three weeks of abdominal pain, nausea and dry heaving. She reported months of joint pain and unintentional weight loss of over 10 pounds within one month. Her bowel movements were normal without diarrhea or bleeding. Family history revealed an aunt with rheumatoid arthritis. Vital signs were normal and labs were notable for a white count of 2.9 k/mm3 and a hemoglobin of 9.3 gm/dL. Computed tomography angiogram (CTA) of the abdomen and pelvis demonstrated normal vasculature and thickening of the small bowel, cecum and ascending colon consistent with enterocolitis. Esophagogastroduodenoscopy and colonoscopy showed normal mucosa without inflammation and normal colonic biopsies. Autoimmune labs were sent for concern for lupus enteritis and revealed low complement C3 (45 mg/dl) and C4 (3 mg/dl). Antinuclear antibody was > 1:1280, anti-smith antibodies > 8.0 and anti-ribonucleic acid antibodies were elevated at 7.3. These findings were consistent with lupus enterocolitis and after discussion with rheumatology, she was started on intravenous (IV) pulse steroids for three days followed by an oral prednisone regimen with marked improvement in her symptoms. She was discharged on prednisone and hydroxychloroquine with rheumatology follow-up.
Discussion: Lupus enterocolitis is a rare entity that commonly presents with abdominal pain and bowel wall thickening on CT. Diagnosis is usually made based on imaging findings, labs consistent with SLE and ruling out inflammatory bowel disease (IBD) on endoscopy. The classic findings on cross sectional imaging includes a target sign in the inflamed bowel segment and occasionally the comb sign suggesting mesenteric edema. Anti-smith antibodies are highly specific for SLE. A high degree of clinical suspicion is required for diagnosis as bowel involvement is an uncommon initial presentation for SLE. In our patient, the suspicion stemmed from the appearance of her small bowel on CT, rheumatologic symptoms and lack of IBD. Initial treatment consists of high dose IV steroids as oral steroids can be poorly absorbed in the setting of bowel edema.

Figure: Image 1: Presence of target sign in the inflamed bowel segment on computed tomography angiogram
Disclosures:
Victoria Caruso indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Victoria A. Caruso, DO1, Muhammad Khan, MD2, Kevin Groudan, MD3, Nha Duong, DO2. P1537 - Lupus Enteritis: An Uncommon Presentation of Lupus Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
