Sunday Poster Session
Category: Small Intestine
P1538 - Duodenal Ampullar Adenocarcinoma: A Case of a Young Female Requiring Pancreaticoduodenectomy (Whipple’s Procedure)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rachael Hagen, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Akaash Mittal, MD2, Neil D.. Parikh, MD3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford Hospital, Harford, CT
Introduction: Duodenal cancer is rare, accounting for 0.35% of gastrointestinal cancers. It carries a 1-, 2-, and 5-year survival rate after surgery of approximately 83.9%, 66.7%, and 51.2%, respectively. Risk factors include Familial Adenomatous Polyposis, Lynch syndrome, Celiac disease, and Crohn’s disease. Here, we present a case of a young female with no known risk factors who was found to have duodenal ampullary adenocarcinoma (DAA).
Case Description/Methods: A 29-year-old female with minimal past medical history presented with three days of right upper quadrant (RUQ) abdominal pain, nausea, and vomiting. Vital signs were unremarkable. Physical exam was remarkable for RUQ tenderness. Laboratory results revealed no leukocytosis, a normal lipase and bilirubin, and elevated liver enzymes.
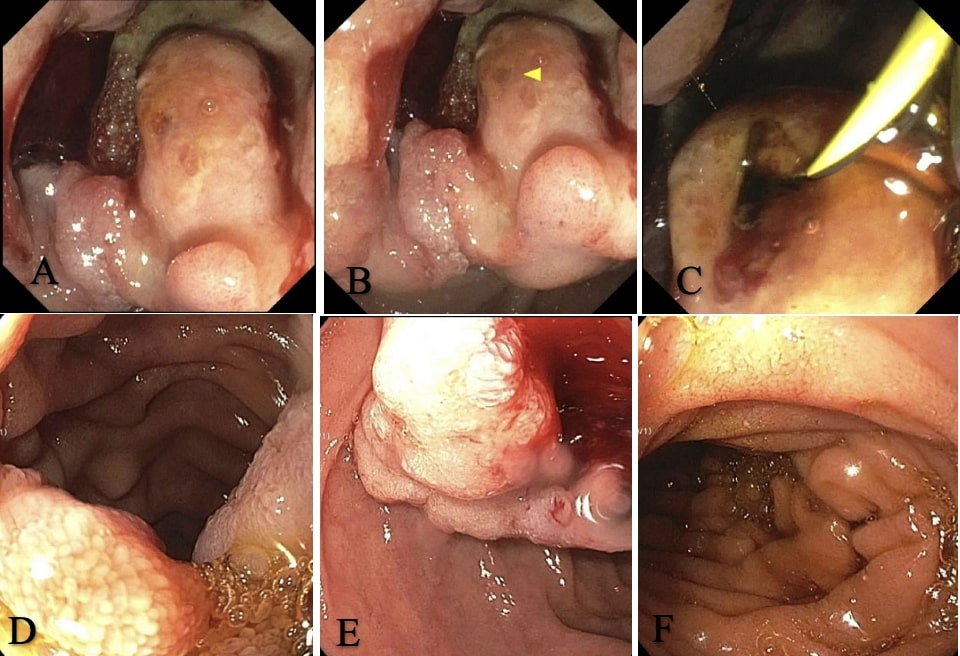
RUQ ultrasound demonstrated a mildly dilated common bile duct (CBD) at 9-mm without cholelithiasis. Magnetic retrograde cholangiopancreatography showed a mildly dilated CBD without choledocholithiasis. HIDA scan was negative for cholecystitis. Endoscopic gastroduodenoscopy (EGD) showed a medium-sized polypoid mass in the duodenum. She was diagnosed with stage T3N0 DAA arising from a tubulovillous adenoma, as no metastases were seen on imaging. Colonoscopy showed a normal-appearing colon. She reported no family history of cancer, and genetic testing ruled out hereditary causes. Endoscopic cholangiopancreatography revealed malignant biliary strictures requiring sphincterotomy and stent placement. She underwent a pancreaticoduodenectomy, with repeat imaging every six months.
Discussion: DAAs are diagnosed via upper endoscopy and management includes pancreaticoduodenectomy. While most DAAs are sporadic, some, particularly in younger patients, are associated with hereditary or inflammatory conditions, warranting genetic testing and colonoscopy as part of the workup. The role of chemotherapy and radiation are unclear. Lymph node metastasis is the most important prognostic factor, which was not seen in this patient. Most patients are diagnosed in the 5th to 7th decade of life, with a median age of 59-64 years. To our knowledge, this is the youngest patient reported in the literature and she had no identifiable risk factors. This patient’s presentation was initially concerning for biliary pain, highlighting the importance of considering endoscopic evaluation of abdominal pain, even in younger patients. DAAs tend to have delayed diagnoses, thus a high index of suspicion is crucial to prompt diagnosis and improve survival outcomes.
Disclosures:
Rachael Hagen, DO1, Akaash Mittal, MD2, Neil D.. Parikh, MD3. P1538 - Duodenal Ampullar Adenocarcinoma: A Case of a Young Female Requiring Pancreaticoduodenectomy (Whipple’s Procedure), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford Hospital, Harford, CT
Introduction: Duodenal cancer is rare, accounting for 0.35% of gastrointestinal cancers. It carries a 1-, 2-, and 5-year survival rate after surgery of approximately 83.9%, 66.7%, and 51.2%, respectively. Risk factors include Familial Adenomatous Polyposis, Lynch syndrome, Celiac disease, and Crohn’s disease. Here, we present a case of a young female with no known risk factors who was found to have duodenal ampullary adenocarcinoma (DAA).
Case Description/Methods: A 29-year-old female with minimal past medical history presented with three days of right upper quadrant (RUQ) abdominal pain, nausea, and vomiting. Vital signs were unremarkable. Physical exam was remarkable for RUQ tenderness. Laboratory results revealed no leukocytosis, a normal lipase and bilirubin, and elevated liver enzymes.
RUQ ultrasound demonstrated a mildly dilated common bile duct (CBD) at 9-mm without cholelithiasis. Magnetic retrograde cholangiopancreatography showed a mildly dilated CBD without choledocholithiasis. HIDA scan was negative for cholecystitis. Endoscopic gastroduodenoscopy (EGD) showed a medium-sized polypoid mass in the duodenum. She was diagnosed with stage T3N0 DAA arising from a tubulovillous adenoma, as no metastases were seen on imaging. Colonoscopy showed a normal-appearing colon. She reported no family history of cancer, and genetic testing ruled out hereditary causes. Endoscopic cholangiopancreatography revealed malignant biliary strictures requiring sphincterotomy and stent placement. She underwent a pancreaticoduodenectomy, with repeat imaging every six months.
Discussion: DAAs are diagnosed via upper endoscopy and management includes pancreaticoduodenectomy. While most DAAs are sporadic, some, particularly in younger patients, are associated with hereditary or inflammatory conditions, warranting genetic testing and colonoscopy as part of the workup. The role of chemotherapy and radiation are unclear. Lymph node metastasis is the most important prognostic factor, which was not seen in this patient. Most patients are diagnosed in the 5th to 7th decade of life, with a median age of 59-64 years. To our knowledge, this is the youngest patient reported in the literature and she had no identifiable risk factors. This patient’s presentation was initially concerning for biliary pain, highlighting the importance of considering endoscopic evaluation of abdominal pain, even in younger patients. DAAs tend to have delayed diagnoses, thus a high index of suspicion is crucial to prompt diagnosis and improve survival outcomes.
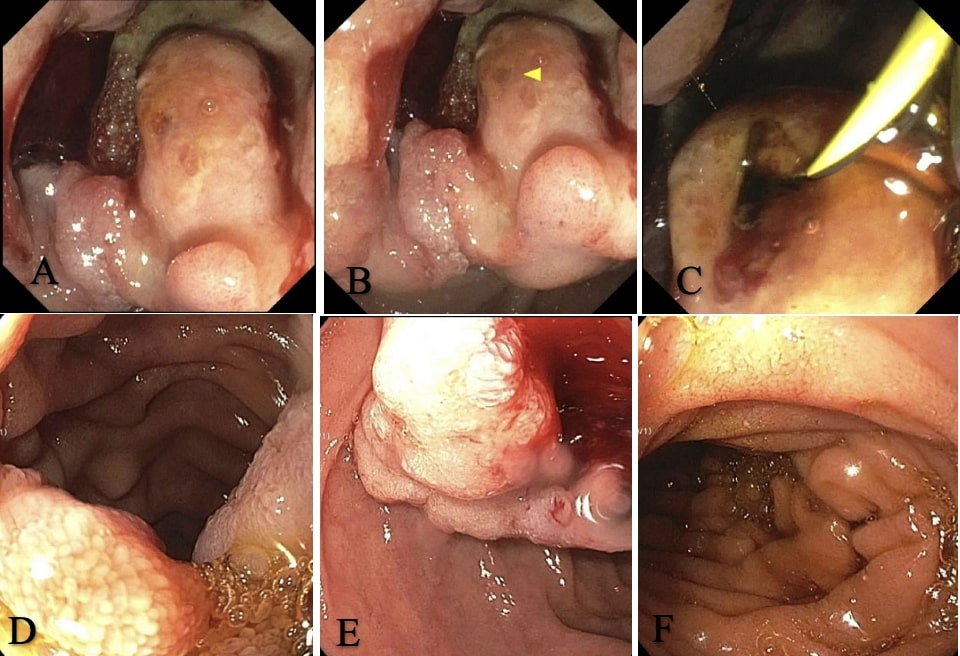
Figure: Figure 1. EGD showed a duodenal polypoid mass in the second portion of duodenum (a) with bleeding (b) which was also seen in the third portion of duodenum (c). ERCP showed an ulcerated cavity in second part of duodenum (d), bleeding in the duodenum ampullary opening (e), and malignant biliary strictures (f).
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Akaash Mittal indicated no relevant financial relationships.
Neil Parikh indicated no relevant financial relationships.
Rachael Hagen, DO1, Akaash Mittal, MD2, Neil D.. Parikh, MD3. P1538 - Duodenal Ampullar Adenocarcinoma: A Case of a Young Female Requiring Pancreaticoduodenectomy (Whipple’s Procedure), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
