Sunday Poster Session
Category: Small Intestine
P1545 - A Former Dancer Regains Some Balance by Avoiding Gluten
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Paola M. Matos Ruiz, BS
Beth Israel Deaconess Medical Center, Harvard Medical School
Somerville, MA
Presenting Author(s)
Award: Presidential Poster Award
Paola Matos Ruiz, BS, Javier A Villafuerte-Galvez, MD
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Gluten ataxia (GA) is a rare extraintestinal manifestation in CeD and non-celiac gluten sensitivity. Elevated CeD serologies have been correlated with worsened cerebellar MRI findings and ataxia severity.
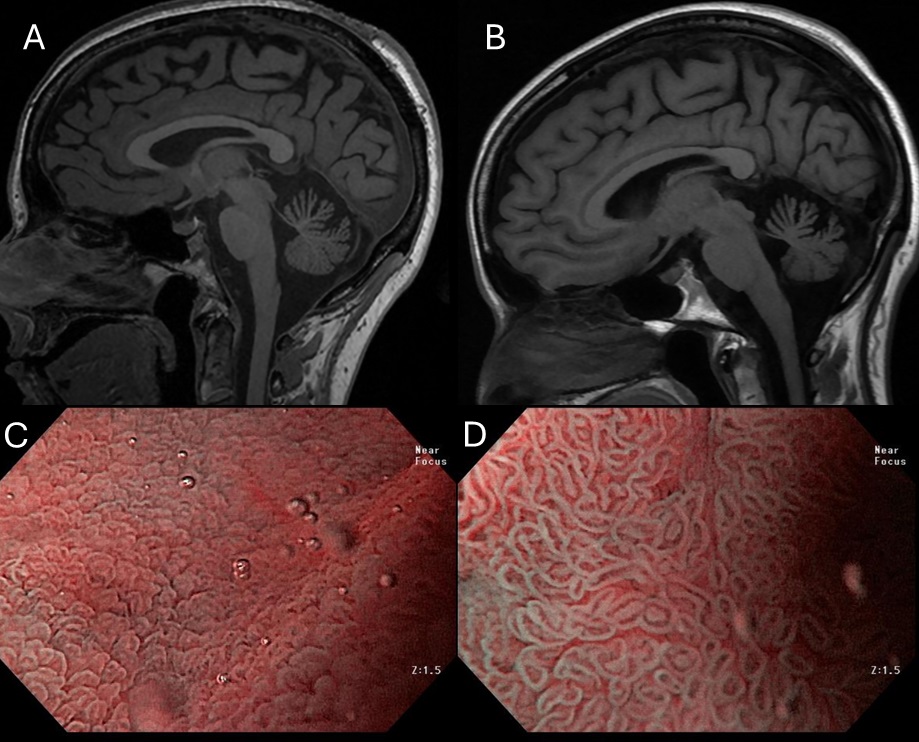
Case Description/Methods: We report the case of a 49-year-old female former dancer with progressive ataxia and new diagnosis of celiac disease (CeD) without gastrointestinal complaints. Twelve years ago, she began with poor balance and progressive loss of core strength responding only partially to physical therapy. Ten years later, she developed in addition blurry vision and declining fine motor skills. Cerebral magnetic resonance imaging (MRI) was significant for vermis-predominant cerebellar atrophy [Panel A]. Extensive workup for vascular, immune, environmental, and genetic causes of ataxia by an ataxia expert was negative, except for Friedriech’s ataxia expansion carrier status deemed unrelated to her current presentation. Subsequent additional testing returned positive elevated CeD serologies (i.e., tTG IgA 2.2x ULN and DGP IgA 2.5x ULN) and heterozygosity for HLA DQ2.5. EGD was significant for conspicuous endoscopic duodenal villous atrophy [Panel C] which biopsies confirmed (subtotal villous atrophy and increased intraepithelial lymphocytes). She then started a gluten free diet (GFD) with subsequent improvement in neurological symptoms (balance, coordination, and nystagmus) and normalization of CeD serologies. However, rapid tandem and ambulation down the stairs remained challenging. A repeat EGD and MRI brain fifteen months after starting GFD, showed resolution of villous atrophy [Panel D] and no progression of cerebellar atrophy [Panel B]. Her ataxia continued to improve clinically with ability to ambulate independently at level. Nonetheless, given persistent difficulty with ambulation up or downstairs her neurologist recommended initiation of a 6-month IVIg.
Discussion: This case reflects on the importance of early diagnosis and treatment to halt or delay the progression of GA.
Disclosures:
Paola Matos Ruiz, BS, Javier A Villafuerte-Galvez, MD. P1545 - A Former Dancer Regains Some Balance by Avoiding Gluten, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Paola Matos Ruiz, BS, Javier A Villafuerte-Galvez, MD
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Gluten ataxia (GA) is a rare extraintestinal manifestation in CeD and non-celiac gluten sensitivity. Elevated CeD serologies have been correlated with worsened cerebellar MRI findings and ataxia severity.
Case Description/Methods: We report the case of a 49-year-old female former dancer with progressive ataxia and new diagnosis of celiac disease (CeD) without gastrointestinal complaints. Twelve years ago, she began with poor balance and progressive loss of core strength responding only partially to physical therapy. Ten years later, she developed in addition blurry vision and declining fine motor skills. Cerebral magnetic resonance imaging (MRI) was significant for vermis-predominant cerebellar atrophy [Panel A]. Extensive workup for vascular, immune, environmental, and genetic causes of ataxia by an ataxia expert was negative, except for Friedriech’s ataxia expansion carrier status deemed unrelated to her current presentation. Subsequent additional testing returned positive elevated CeD serologies (i.e., tTG IgA 2.2x ULN and DGP IgA 2.5x ULN) and heterozygosity for HLA DQ2.5. EGD was significant for conspicuous endoscopic duodenal villous atrophy [Panel C] which biopsies confirmed (subtotal villous atrophy and increased intraepithelial lymphocytes). She then started a gluten free diet (GFD) with subsequent improvement in neurological symptoms (balance, coordination, and nystagmus) and normalization of CeD serologies. However, rapid tandem and ambulation down the stairs remained challenging. A repeat EGD and MRI brain fifteen months after starting GFD, showed resolution of villous atrophy [Panel D] and no progression of cerebellar atrophy [Panel B]. Her ataxia continued to improve clinically with ability to ambulate independently at level. Nonetheless, given persistent difficulty with ambulation up or downstairs her neurologist recommended initiation of a 6-month IVIg.
Discussion: This case reflects on the importance of early diagnosis and treatment to halt or delay the progression of GA.
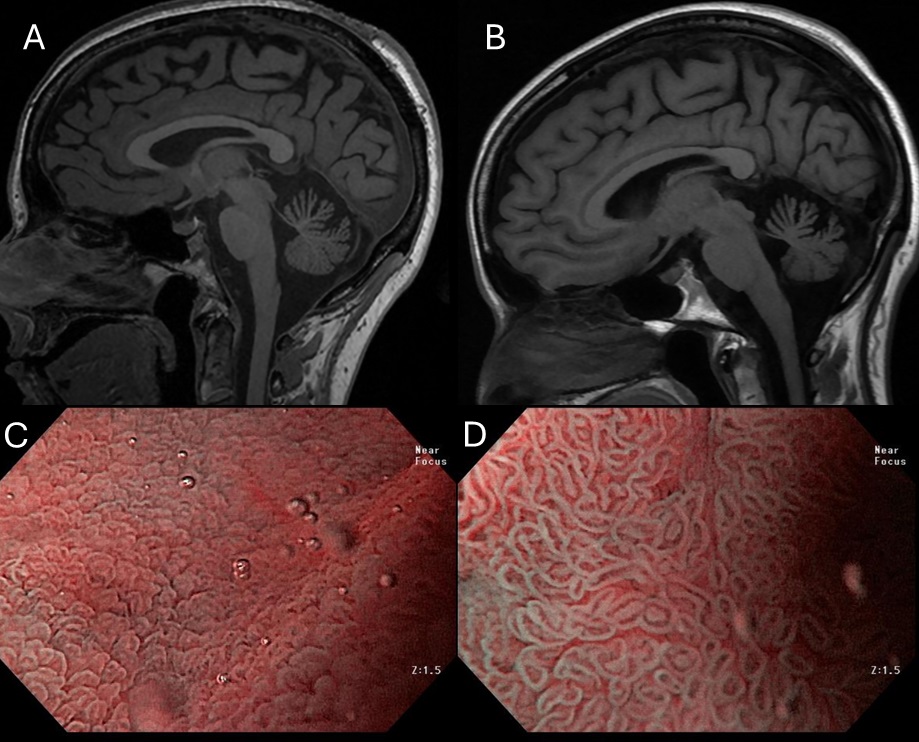
Figure: Legend: (A) MRI brain in 2020 with vermis-predominant cerebellar atrophy; (B) Halted progression of cerebellar atrophy at interval MRI in 2024, 15 months into GFD; (C) Marked villous shortening in the duodenal bulb at the time of diagnosis of CeD; (D) Normalization of villi 15 months into GFD
Disclosures:
Paola Matos Ruiz indicated no relevant financial relationships.
Javier A Villafuerte-Galvez indicated no relevant financial relationships.
Paola Matos Ruiz, BS, Javier A Villafuerte-Galvez, MD. P1545 - A Former Dancer Regains Some Balance by Avoiding Gluten, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

