Sunday Poster Session
Category: Obesity
P1437 - GLP-1 Agonist Use is Associated With Lower Incidence of GERD, Lower Use of PPIs and Does Not Complicate GERD in Patients With Obesity Who Undergo Sleeve Gastrectomy: A National Database Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Luis M. Nieto, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Sharon Narvaez, MD1, Luis M.. Nieto, MD2, Olanrewaju Adeniran, MBBS3, Donghyun Ko, MD4, Do Han Kim, MD5, Kenneth Vega, MD, FACG6, Treah Haggerty, MD3, Laura Davisson, MD3, Lawrence Tabone, MD3, Saurabh Chawla, MD2
1Universidad de Guayaquil, School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA; 3West Virginia University, Morgantown, WV; 4Yale-New Haven Health/Bridgeport Hospital, Bridgeport, CT; 5Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 6Medical College of Georgia at Augusta University, Augusta, GA
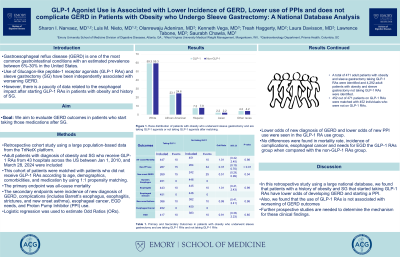
Introduction: Gastroesophageal reflux disease (GERD) is one of the most common gastrointestinal conditions with an estimated prevalence between 6%-30% in the United States. Use of Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sleeve gastrectomy (SG) have been independently associated with worsening GERD. However, there is a paucity of data related to the esophageal impact after starting GLP-1 RAs in patients with obesity and history of SG. Therefore, we aim to evaluate GERD outcomes in patients who start taking those medications after SG.
Methods: We performed a retrospective cohort study utilizing large population-based data from the TriNetX platform. We identified patients older than 18 with a history of obesity and SG before starting GLP-1 RAs (semaglutide, liraglutide, dulaglutide and tirzepatide) between January 1, 2010, and March 28, 2024. This cohort was matched with patients with a history of obesity and SG who did not receive GLP-1 RAs according to age, demographics, comorbidities, and medication by using 1:1 propensity matching. The primary endpoint was all-cause mortality, and the secondary endpoints were incidence of new diagnosis of GERD, complications (includes Barrett’s esophagus, esophagitis, strictures, and new onset asthma), esophageal cancer, EGD needs, and Proton Pump Inhibitor (PPI) use. Logistic regression was used to estimate odd ratios (ORs).
Results: A total of 4,763 adult patients with history of obesity and SG were identified, 471 of these individuals received GLP -1 RAs at some point after the procedure; 452 out of 471 (mean [SD] age, 46.6 [11.8] years; 359 [79.43%] female) were matched with 452 individuals (mean [SD] age, 46.2 [14.2] years; 361 [79.87 %] female) who did not received GLP-1 RAs. See table 1-2. The GLP-1 RAs group had significantly lower odds of new diagnosis of GERD (ORs, 0.51; 95% Confidence Interval [CI], 0.26-0.99) and lower odds of new PPI use (ORs, 0.37; 95% CI, 0.19-0.70). No differences were found in mortality rate, incidence of complications, esophageal cancer, and needs for EGD.
Discussion: In this retrospective study using a large national database, we found that patients with a history of obesity and SG that started taking GLP-1 RAs have lower odds of developing GERD and starting a PPI. Also, we found that the use of GLP-1 RAs is not associated with worsening of GERD outcomes. Further prospective studies are needed to determine the mechanism for these clinical findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sharon Narvaez, MD1, Luis M.. Nieto, MD2, Olanrewaju Adeniran, MBBS3, Donghyun Ko, MD4, Do Han Kim, MD5, Kenneth Vega, MD, FACG6, Treah Haggerty, MD3, Laura Davisson, MD3, Lawrence Tabone, MD3, Saurabh Chawla, MD2. P1437 - GLP-1 Agonist Use is Associated With Lower Incidence of GERD, Lower Use of PPIs and Does Not Complicate GERD in Patients With Obesity Who Undergo Sleeve Gastrectomy: A National Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Universidad de Guayaquil, School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA; 3West Virginia University, Morgantown, WV; 4Yale-New Haven Health/Bridgeport Hospital, Bridgeport, CT; 5Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 6Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Gastroesophageal reflux disease (GERD) is one of the most common gastrointestinal conditions with an estimated prevalence between 6%-30% in the United States. Use of Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sleeve gastrectomy (SG) have been independently associated with worsening GERD. However, there is a paucity of data related to the esophageal impact after starting GLP-1 RAs in patients with obesity and history of SG. Therefore, we aim to evaluate GERD outcomes in patients who start taking those medications after SG.
Methods: We performed a retrospective cohort study utilizing large population-based data from the TriNetX platform. We identified patients older than 18 with a history of obesity and SG before starting GLP-1 RAs (semaglutide, liraglutide, dulaglutide and tirzepatide) between January 1, 2010, and March 28, 2024. This cohort was matched with patients with a history of obesity and SG who did not receive GLP-1 RAs according to age, demographics, comorbidities, and medication by using 1:1 propensity matching. The primary endpoint was all-cause mortality, and the secondary endpoints were incidence of new diagnosis of GERD, complications (includes Barrett’s esophagus, esophagitis, strictures, and new onset asthma), esophageal cancer, EGD needs, and Proton Pump Inhibitor (PPI) use. Logistic regression was used to estimate odd ratios (ORs).
Results: A total of 4,763 adult patients with history of obesity and SG were identified, 471 of these individuals received GLP -1 RAs at some point after the procedure; 452 out of 471 (mean [SD] age, 46.6 [11.8] years; 359 [79.43%] female) were matched with 452 individuals (mean [SD] age, 46.2 [14.2] years; 361 [79.87 %] female) who did not received GLP-1 RAs. See table 1-2. The GLP-1 RAs group had significantly lower odds of new diagnosis of GERD (ORs, 0.51; 95% Confidence Interval [CI], 0.26-0.99) and lower odds of new PPI use (ORs, 0.37; 95% CI, 0.19-0.70). No differences were found in mortality rate, incidence of complications, esophageal cancer, and needs for EGD.
Discussion: In this retrospective study using a large national database, we found that patients with a history of obesity and SG that started taking GLP-1 RAs have lower odds of developing GERD and starting a PPI. Also, we found that the use of GLP-1 RAs is not associated with worsening of GERD outcomes. Further prospective studies are needed to determine the mechanism for these clinical findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sharon Narvaez indicated no relevant financial relationships.
Luis Nieto indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Donghyun Ko indicated no relevant financial relationships.
Do Han Kim indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Treah Haggerty indicated no relevant financial relationships.
Laura Davisson indicated no relevant financial relationships.
Lawrence Tabone indicated no relevant financial relationships.
Saurabh Chawla indicated no relevant financial relationships.
Sharon Narvaez, MD1, Luis M.. Nieto, MD2, Olanrewaju Adeniran, MBBS3, Donghyun Ko, MD4, Do Han Kim, MD5, Kenneth Vega, MD, FACG6, Treah Haggerty, MD3, Laura Davisson, MD3, Lawrence Tabone, MD3, Saurabh Chawla, MD2. P1437 - GLP-1 Agonist Use is Associated With Lower Incidence of GERD, Lower Use of PPIs and Does Not Complicate GERD in Patients With Obesity Who Undergo Sleeve Gastrectomy: A National Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
