Sunday Poster Session
Category: Obesity
P1450 - Trends in Malnutrition-Related Mortality in the United States, 1999-2020: An Epidemiological Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MK
Muhammad Ali Khaqan, MD
John H. Stroger, Jr. Hospital of Cook County
Lexington, KY
Presenting Author(s)
Muhammad Ali Khaqan, MD1, Muhammad Shahzil, MD2, Zainab Alvi, MBBS3, Luqman Munir, 3, Ali Akram Qureshi, 3, Syed Adeel Hassan, MD4, Terrence Barrett, MD4
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 3King Edward Medical University, Lahore, Punjab, Pakistan; 4University of Kentucky, Lexington, KY
Introduction: Over the past two decades, malnutrition-related mortality in the United States has shown a troubling increase, posing significant public health challenges exacerbated by socio-economic disparities and systemic inequities. This study analyzes trends from 1999 to 2020 using age-adjusted mortality rates (AAMR) to understand patterns across demographics and regions.
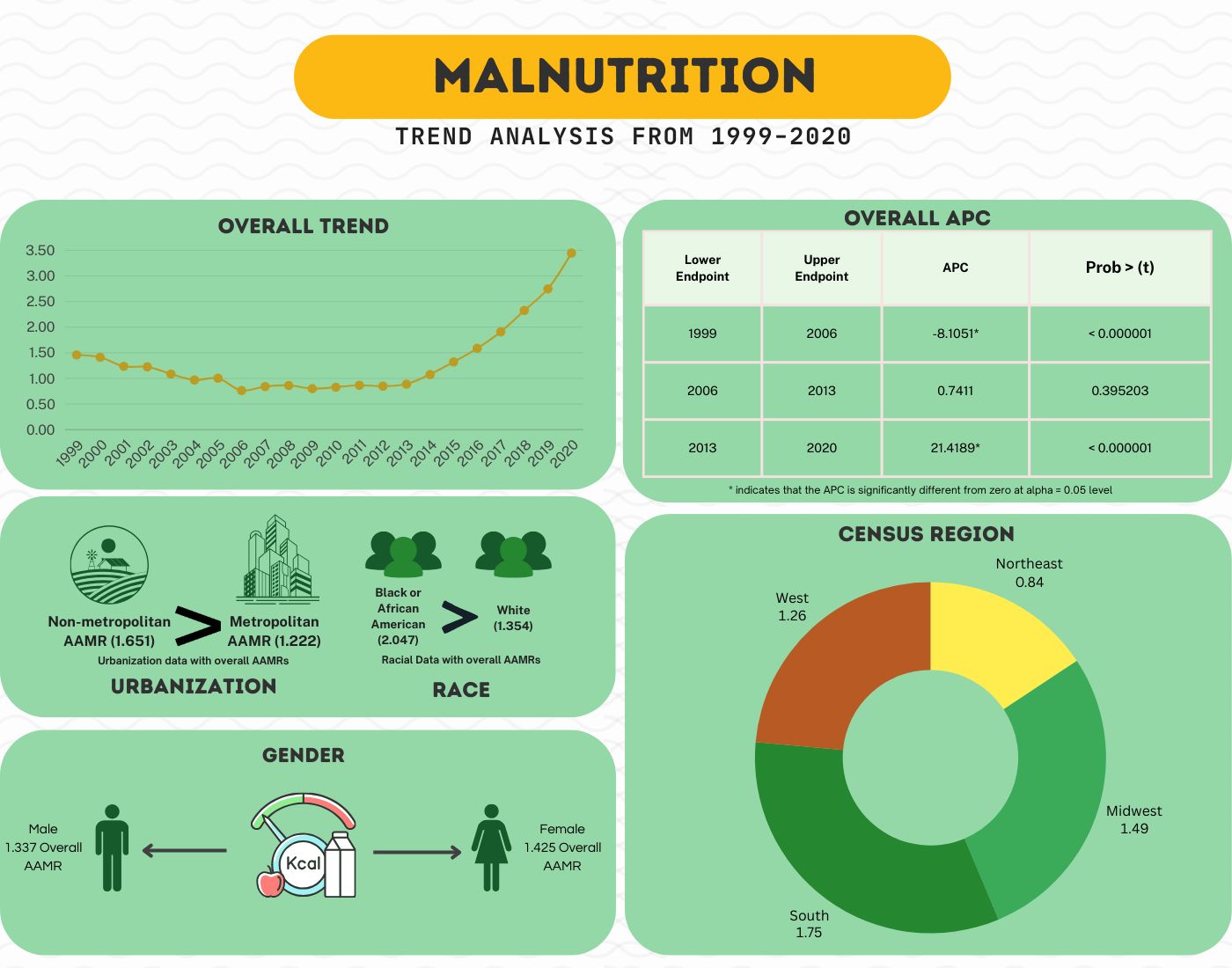
Methods: Data from the CDC WONDER database were analyzed for malnutrition-related deaths from January 1, 1999, to December 31, 2020, across all age groups. We calculated age-adjusted mortality rates (AAMRs) per 100,000 population and the average annual percentage change (AAPC). Annual percentage changes (APCs) with 95% confidence intervals were assessed to understand AAMR trends using Joinpoint regression analysis. The Monte Carlo Permutation Procedure (MCPP) analyzed mortality trends. Statistically significant results were determined by a p-value < 0.05, using a two-sided t-test against a null value of 0.
Results: The analysis included 103,962 malnutrition-related deaths over the study period. After a decrease in age-adjusted mortality rate (AAMR) from 1999 to 2006, rates plateaued until 2013, then rose, reaching 3.449 in 2020. Higher AAMRs were seen among females (1.425), African Americans (2.047), non-metropolitan residents (1.651), and the Southern region (1.75). The average annual percent change (AAPC) for overall mortality was 3.9748. APC analysis showed a decline from 1999 to 2006 (APC -8.1051), stabilization from 2006 to 2013, and acceleration from 2013 to 2020 (APC 21.4189). Lower AAMRs were found in metropolitan areas (1.222) compared to non-metropolitan (1.539). The 85+ age group had the highest AAMR (199.6) and a significant recent rise. African Americans had substantially higher AAMRs (2.047) than Whites (1.354).
Discussion: Analysis of 22 years shows alarming malnutrition-related mortality disparities in the US across ethnicities, gender, urbanization, and regions. Urgent public health action is needed to address systemic inequities through enhanced food security, healthcare access, and socio-economic support to curb rising death rates.
Disclosures:
Muhammad Ali Khaqan, MD1, Muhammad Shahzil, MD2, Zainab Alvi, MBBS3, Luqman Munir, 3, Ali Akram Qureshi, 3, Syed Adeel Hassan, MD4, Terrence Barrett, MD4. P1450 - Trends in Malnutrition-Related Mortality in the United States, 1999-2020: An Epidemiological Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 3King Edward Medical University, Lahore, Punjab, Pakistan; 4University of Kentucky, Lexington, KY
Introduction: Over the past two decades, malnutrition-related mortality in the United States has shown a troubling increase, posing significant public health challenges exacerbated by socio-economic disparities and systemic inequities. This study analyzes trends from 1999 to 2020 using age-adjusted mortality rates (AAMR) to understand patterns across demographics and regions.
Methods: Data from the CDC WONDER database were analyzed for malnutrition-related deaths from January 1, 1999, to December 31, 2020, across all age groups. We calculated age-adjusted mortality rates (AAMRs) per 100,000 population and the average annual percentage change (AAPC). Annual percentage changes (APCs) with 95% confidence intervals were assessed to understand AAMR trends using Joinpoint regression analysis. The Monte Carlo Permutation Procedure (MCPP) analyzed mortality trends. Statistically significant results were determined by a p-value < 0.05, using a two-sided t-test against a null value of 0.
Results: The analysis included 103,962 malnutrition-related deaths over the study period. After a decrease in age-adjusted mortality rate (AAMR) from 1999 to 2006, rates plateaued until 2013, then rose, reaching 3.449 in 2020. Higher AAMRs were seen among females (1.425), African Americans (2.047), non-metropolitan residents (1.651), and the Southern region (1.75). The average annual percent change (AAPC) for overall mortality was 3.9748. APC analysis showed a decline from 1999 to 2006 (APC -8.1051), stabilization from 2006 to 2013, and acceleration from 2013 to 2020 (APC 21.4189). Lower AAMRs were found in metropolitan areas (1.222) compared to non-metropolitan (1.539). The 85+ age group had the highest AAMR (199.6) and a significant recent rise. African Americans had substantially higher AAMRs (2.047) than Whites (1.354).
Discussion: Analysis of 22 years shows alarming malnutrition-related mortality disparities in the US across ethnicities, gender, urbanization, and regions. Urgent public health action is needed to address systemic inequities through enhanced food security, healthcare access, and socio-economic support to curb rising death rates.
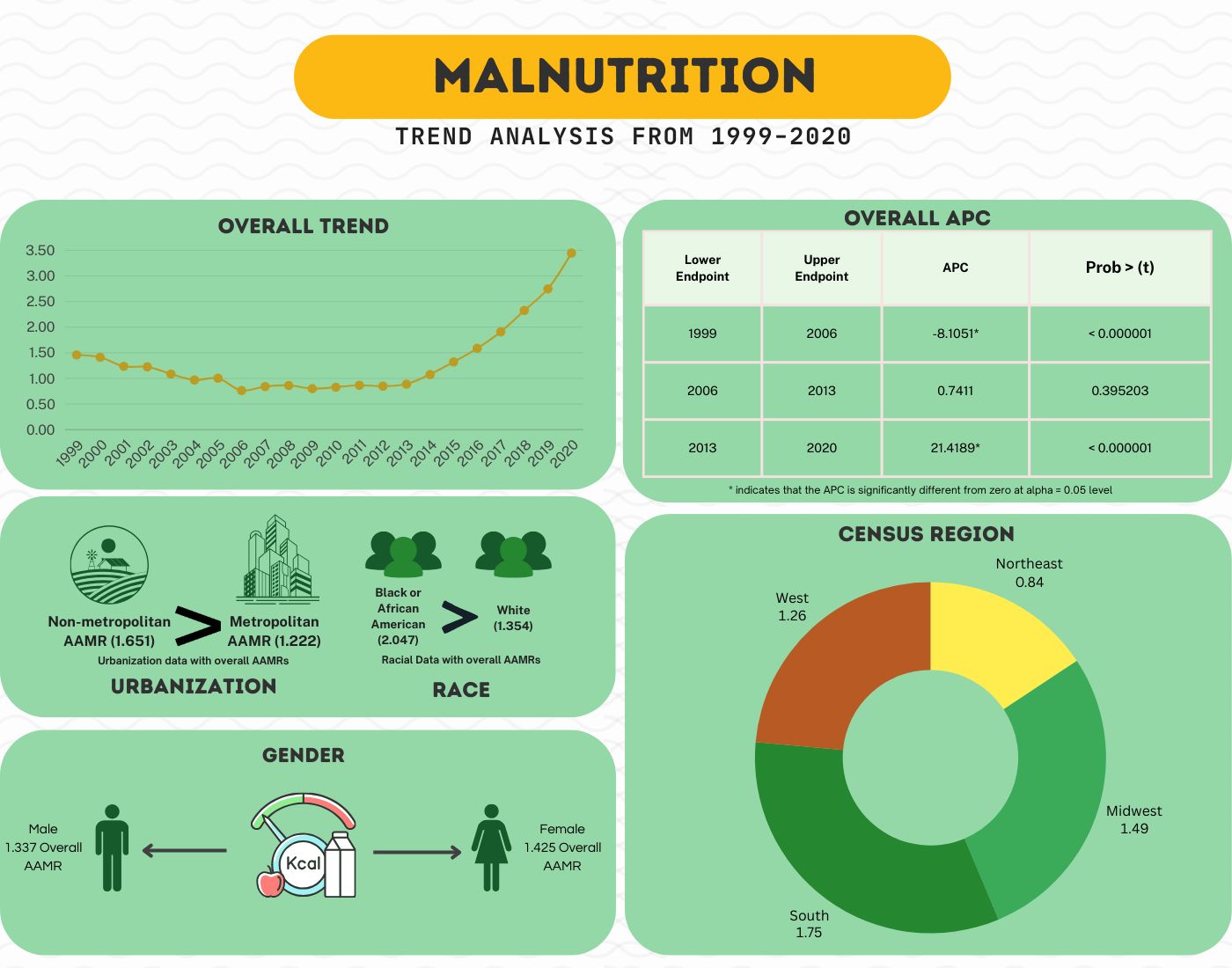
Figure: Trends in Malnutrition-Related Mortality in the United States, 1999-2020: An Epidemiological Analysis
Disclosures:
Muhammad Ali Khaqan indicated no relevant financial relationships.
Muhammad Shahzil indicated no relevant financial relationships.
Zainab Alvi indicated no relevant financial relationships.
Luqman Munir indicated no relevant financial relationships.
Ali Akram Qureshi indicated no relevant financial relationships.
Syed Adeel Hassan indicated no relevant financial relationships.
Terrence Barrett indicated no relevant financial relationships.
Muhammad Ali Khaqan, MD1, Muhammad Shahzil, MD2, Zainab Alvi, MBBS3, Luqman Munir, 3, Ali Akram Qureshi, 3, Syed Adeel Hassan, MD4, Terrence Barrett, MD4. P1450 - Trends in Malnutrition-Related Mortality in the United States, 1999-2020: An Epidemiological Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
