Sunday Poster Session
Category: Liver
P1364 - A Curious Case of Variceal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

William Ghaul, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
William Ghaul, DO1, Cristina Angelo, MD1, Janson Jacob, MD1, Michael Engels, MD2
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Common sources of upper GI bleeding include peptic ulcer disease and arteriovenous malformations. In cirrhotic patients, variceal bleeding must be ruled out. The first diagnostic test of choice is either an endoscopy or CT angiogram. Peristomal varices following an urological procedure are rare. We present a case of a patient with recurrent hematuria from his stoma site refractory to ligation, found to have peristomal varices.
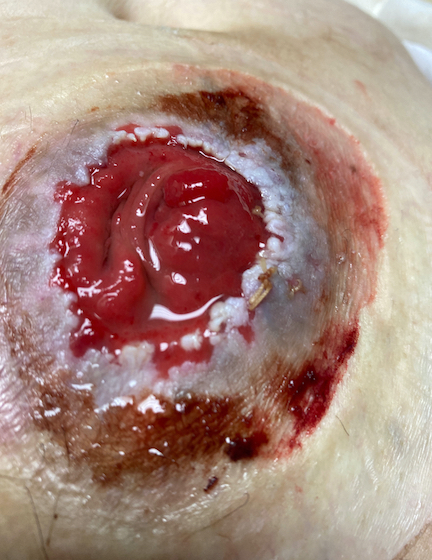
Case Description/Methods: A 76-year-old male with a past medical history of previously well-compensated MASH cirrhosis, bladder cancer s/p radical prostatectomy with ileal conduit, diabetes, and heart failure who presented due to recurrent bleeding from his stomal site. The patient had multiple admissions in the past 2 years prior to arrival for similar. He had previously been treated with ligation/cauterization. Lab work revealed hemoglobin to be at baseline (8.7). Gastroenterology was consulted due to concern for peristomal varices. Physical examination showed evidence of prior bleeding along edges of stomal site. CT with IV contrast revealed a parastomal hernia with a large enhancing vessel/varix measuring 8 mm within the hernia extending to the surface of the skin. He was started on carvedilol. He ultimately underwent sclerotherapy and coil embolization with interventional radiology.
Discussion: Peristomal bleeding is an uncommon etiology of upper gastrointestinal bleeding. Those with portal hypertension are not typically offered stoma formation for this reason. However, in our case, he unfortunately developed MASH cirrhosis following his procedure in 2019. An estimated 5% of patients with surgical stomas and portal hypertension develop peristomal bleeding1. The risk of mortality is 4% in each of these cases1. Treatment is largely supportive with beta blocker prophylaxis. Surgical options for these patients requires more research. Current available options include transjugular intrahepatic portosystemic shunt (TIPS) or coil embolization. However, these procedures increase the risk of hepatic encephalopathy and re-siting of parastomal varices, respectively. Long-term outcomes following these procedures remains unknown.
Disclosures:
William Ghaul, DO1, Cristina Angelo, MD1, Janson Jacob, MD1, Michael Engels, MD2. P1364 - A Curious Case of Variceal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Common sources of upper GI bleeding include peptic ulcer disease and arteriovenous malformations. In cirrhotic patients, variceal bleeding must be ruled out. The first diagnostic test of choice is either an endoscopy or CT angiogram. Peristomal varices following an urological procedure are rare. We present a case of a patient with recurrent hematuria from his stoma site refractory to ligation, found to have peristomal varices.
Case Description/Methods: A 76-year-old male with a past medical history of previously well-compensated MASH cirrhosis, bladder cancer s/p radical prostatectomy with ileal conduit, diabetes, and heart failure who presented due to recurrent bleeding from his stomal site. The patient had multiple admissions in the past 2 years prior to arrival for similar. He had previously been treated with ligation/cauterization. Lab work revealed hemoglobin to be at baseline (8.7). Gastroenterology was consulted due to concern for peristomal varices. Physical examination showed evidence of prior bleeding along edges of stomal site. CT with IV contrast revealed a parastomal hernia with a large enhancing vessel/varix measuring 8 mm within the hernia extending to the surface of the skin. He was started on carvedilol. He ultimately underwent sclerotherapy and coil embolization with interventional radiology.
Discussion: Peristomal bleeding is an uncommon etiology of upper gastrointestinal bleeding. Those with portal hypertension are not typically offered stoma formation for this reason. However, in our case, he unfortunately developed MASH cirrhosis following his procedure in 2019. An estimated 5% of patients with surgical stomas and portal hypertension develop peristomal bleeding1. The risk of mortality is 4% in each of these cases1. Treatment is largely supportive with beta blocker prophylaxis. Surgical options for these patients requires more research. Current available options include transjugular intrahepatic portosystemic shunt (TIPS) or coil embolization. However, these procedures increase the risk of hepatic encephalopathy and re-siting of parastomal varices, respectively. Long-term outcomes following these procedures remains unknown.
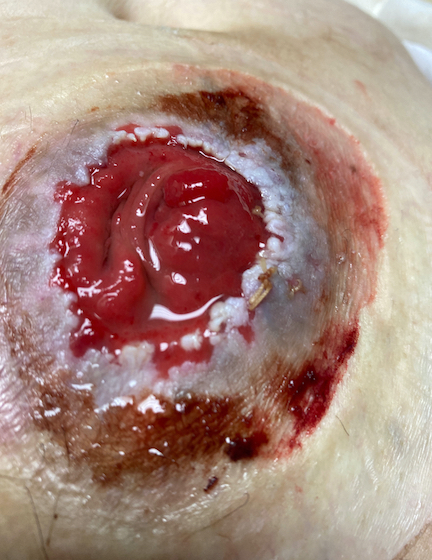
Figure: Figure 1: Bleeding peristomal varices with adhesive dressing removed.
Disclosures:
William Ghaul indicated no relevant financial relationships.
Cristina Angelo indicated no relevant financial relationships.
Janson Jacob indicated no relevant financial relationships.
Michael Engels indicated no relevant financial relationships.
William Ghaul, DO1, Cristina Angelo, MD1, Janson Jacob, MD1, Michael Engels, MD2. P1364 - A Curious Case of Variceal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
