Sunday Poster Session
Category: Liver
P1280 - Hyperammonemia Syndrome After Combined Liver-Kidney Transplantation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AS
Apurva Pravin Shrigiriwar, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Apurva Pravin Shrigiriwar, MD, Bryce Yohannan, MD, Sidra Ahsan, MD
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Hyperammonemia syndrome (HS) due to Ureaplasma infection has been described most commonly in patients who have undergone lung transplantation. Here, we present a case of HS after combined liver-kidney transplant; to our knowledge, this is only the second case of HS after combined liver-kidney transplantation reported in the literature.
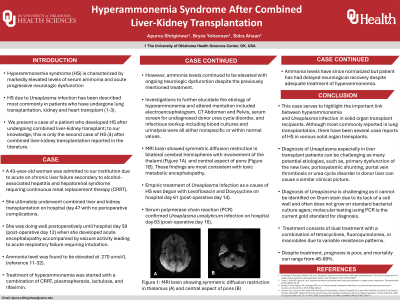
Case Description/Methods: A 43-year-old woman was admitted for acute on chronic liver failure secondary to alcohol-associated hepatitis and hepatorenal syndrome requiring continuous renal replacement therapy (CRRT). She ultimately underwent combined liver and kidney transplantation without perioperative complications. She was doing well postoperatively until hospital day 59 (post-operative day (POD) 12) when she developed acute encephalopathy. Ammonia was elevated at 270 umol/L (reference 11-32). She was treated with a combination of CRRT, plasmapheresis, lactulose, and rifaximin. Investigations to elucidate the etiology of hyperammonemia and altered mentation included MRI Brain, electroencephalogram, CT Abdomen and Pelvis, serum screen for undiagnosed donor urea cycle disorder, and infectious workup including blood cultures and urinalysis were unrevealing. Empiric treatment of Ureaplasma urealyticum infection as a cause of HS was begun with Levofloxacin and Doxycycline on POD 14 with serum polymerase chain reaction (PCR) confirmation on POD 16. Ammonia levels have since normalized but she has had delayed neurological recovery despite adequate treatment.
Discussion: This case serves to highlight the important link between hyperammonemia and Ureaplasma infection in solid organ transplant recipients. Although most commonly reported in lung transplantation, there have been several case reports of HS in various solid organ transplants. However, this is only the second reported case of HS due to Ureaplasma infection in a combined liver-kidney transplant patient. Diagnosis of Ureaplasma is challenging as it cannot be identified on Gram stain due to its lack of a cell wall and often does not grow on standard bacterial culture agars; molecular testing using PCR is the current gold standard for diagnosis. Treatment consists of dual treatment with a combination of tetracyclines, fluoroquinolones, or macrolides due to variable resistance patterns. Despite treatment, prognosis is poor, and mortality can range from 46-69%. Clinicians should have a high index of suspicion for Ureaplasma infection in cases of hyperammonemia after solid organ transplantation.
Disclosures:
Apurva Pravin Shrigiriwar, MD, Bryce Yohannan, MD, Sidra Ahsan, MD. P1280 - Hyperammonemia Syndrome After Combined Liver-Kidney Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Hyperammonemia syndrome (HS) due to Ureaplasma infection has been described most commonly in patients who have undergone lung transplantation. Here, we present a case of HS after combined liver-kidney transplant; to our knowledge, this is only the second case of HS after combined liver-kidney transplantation reported in the literature.
Case Description/Methods: A 43-year-old woman was admitted for acute on chronic liver failure secondary to alcohol-associated hepatitis and hepatorenal syndrome requiring continuous renal replacement therapy (CRRT). She ultimately underwent combined liver and kidney transplantation without perioperative complications. She was doing well postoperatively until hospital day 59 (post-operative day (POD) 12) when she developed acute encephalopathy. Ammonia was elevated at 270 umol/L (reference 11-32). She was treated with a combination of CRRT, plasmapheresis, lactulose, and rifaximin. Investigations to elucidate the etiology of hyperammonemia and altered mentation included MRI Brain, electroencephalogram, CT Abdomen and Pelvis, serum screen for undiagnosed donor urea cycle disorder, and infectious workup including blood cultures and urinalysis were unrevealing. Empiric treatment of Ureaplasma urealyticum infection as a cause of HS was begun with Levofloxacin and Doxycycline on POD 14 with serum polymerase chain reaction (PCR) confirmation on POD 16. Ammonia levels have since normalized but she has had delayed neurological recovery despite adequate treatment.
Discussion: This case serves to highlight the important link between hyperammonemia and Ureaplasma infection in solid organ transplant recipients. Although most commonly reported in lung transplantation, there have been several case reports of HS in various solid organ transplants. However, this is only the second reported case of HS due to Ureaplasma infection in a combined liver-kidney transplant patient. Diagnosis of Ureaplasma is challenging as it cannot be identified on Gram stain due to its lack of a cell wall and often does not grow on standard bacterial culture agars; molecular testing using PCR is the current gold standard for diagnosis. Treatment consists of dual treatment with a combination of tetracyclines, fluoroquinolones, or macrolides due to variable resistance patterns. Despite treatment, prognosis is poor, and mortality can range from 46-69%. Clinicians should have a high index of suspicion for Ureaplasma infection in cases of hyperammonemia after solid organ transplantation.
Disclosures:
Apurva Pravin Shrigiriwar indicated no relevant financial relationships.
Bryce Yohannan indicated no relevant financial relationships.
Sidra Ahsan indicated no relevant financial relationships.
Apurva Pravin Shrigiriwar, MD, Bryce Yohannan, MD, Sidra Ahsan, MD. P1280 - Hyperammonemia Syndrome After Combined Liver-Kidney Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
