Sunday Poster Session
Category: Liver
P1281 - Unveiling the Mystery of Veins: A Unique Combination of Portal and Inferior Mesenteric Venous Thrombosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Majd Khadra, MD
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Rida Farook, BS2, Camila Arellano, BS2, Naveed Shaikh, MD3
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State School of Medicine, Detroit, MI; 3John D. Dingell VA Medical Center, Detroit, MI
Introduction: Patients with portal vein thrombosis (PVT) classically have liver cirrhosis but may also have an inherited or acquired condition that increases their hypercoagulability. PVT and mesenteric vein thrombosis can occur simultaneously. Typically, PVT is more commonly associated with superior mesenteric vein (SMV) thrombosis rather than Inferior mesenteric vein (IMV) thrombosis.
Case Description/Methods: A 75-year-old male with a history of hyperlipidemia and type 2 diabetes mellitus presented to the emergency department (ED) with severe, sudden, sharp periumbilical pain that was relieved with intravenous morphine. In the ED, the patient was hemodynamically stable with lab findings of platelets 200k platelets/mcL, Lactic acid 1 mmol/L, Total Bilirubin 0.2 mg/dL, Alkaline Phosphatase (ALK-P ) 60 U/L, Alanine Aminotransferase (ALT) 55 U/L, Aspartate Aminotransferase (AST) 65 U/L, Prothrombin Time (PT) 12 seconds, International Normalized Ratio (INR) 0.9, Activated Partial Thromboplastin Time (aPTT) 27 seconds, Fibrinogen 300 mg/dL, D-Dimer 200 ng/mL.
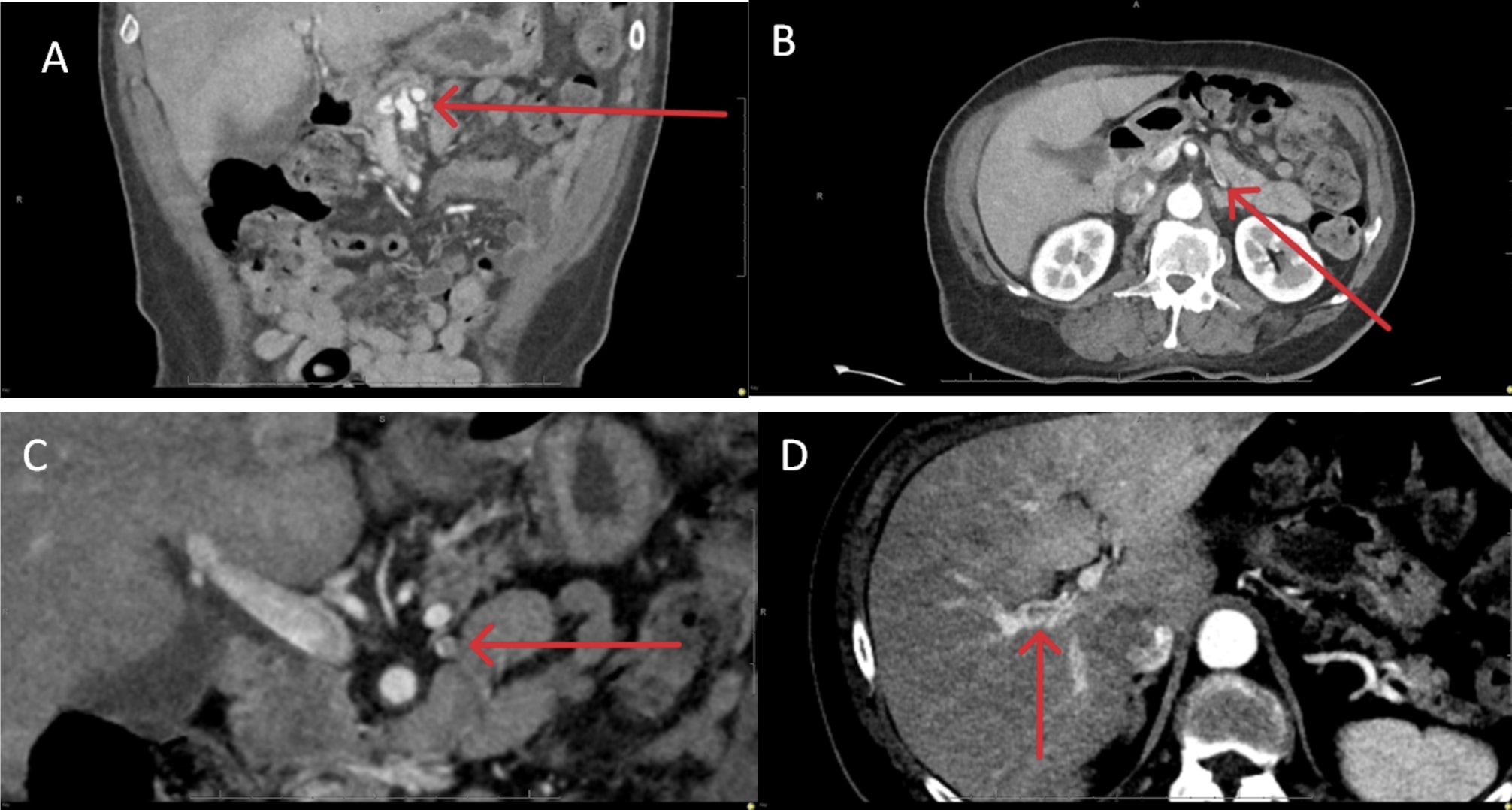
Computed tomography (CT) of the abdomen and pelvis (Figure 1) was ordered which showed a thrombus within the inferior mesenteric vein (IMV) and the proximal branch of the right portal vein. Vascular surgery was consulted in the ED to assess for any acute intervention. However, given the CT abdomen and pelvis report and the normal lactic acid level, no acute intervention was needed. The patient was then admitted to medicine for hypercoagulability workup. Patient denied any family history of blood clotting disorders. He was started on intramuscular Lovenox 70 mg injection twice daily. Gastroenterology was consulted and recommended to trend liver function test. Hematology was consulted and recommended ordering (anticardiolipin antibodies, lupus anticoagulant, anti-beta-2-GPI antibodies, Factor V Leiden, Prothrombin gene, Antithrombin III, Homocysteine, protein C, and protein S) that were all negative for abnormalities. The patient’s pain and labs improved over the next couple of days, and was discharged on apixaban 10 mg twice daily for 7 days followed by 5 mg twice daily.
Discussion: This case highlights the unusual occurrence of concurrent thrombosis in the inferior mesenteric vein (IMV) and portal vein (PVT), emphasizing the importance of maintaining a high level of suspicion for thromboses in uncommon locations when patients present with abdominal pain.
Disclosures:
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Rida Farook, BS2, Camila Arellano, BS2, Naveed Shaikh, MD3. P1281 - Unveiling the Mystery of Veins: A Unique Combination of Portal and Inferior Mesenteric Venous Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State School of Medicine, Detroit, MI; 3John D. Dingell VA Medical Center, Detroit, MI
Introduction: Patients with portal vein thrombosis (PVT) classically have liver cirrhosis but may also have an inherited or acquired condition that increases their hypercoagulability. PVT and mesenteric vein thrombosis can occur simultaneously. Typically, PVT is more commonly associated with superior mesenteric vein (SMV) thrombosis rather than Inferior mesenteric vein (IMV) thrombosis.
Case Description/Methods: A 75-year-old male with a history of hyperlipidemia and type 2 diabetes mellitus presented to the emergency department (ED) with severe, sudden, sharp periumbilical pain that was relieved with intravenous morphine. In the ED, the patient was hemodynamically stable with lab findings of platelets 200k platelets/mcL, Lactic acid 1 mmol/L, Total Bilirubin 0.2 mg/dL, Alkaline Phosphatase (ALK-P ) 60 U/L, Alanine Aminotransferase (ALT) 55 U/L, Aspartate Aminotransferase (AST) 65 U/L, Prothrombin Time (PT) 12 seconds, International Normalized Ratio (INR) 0.9, Activated Partial Thromboplastin Time (aPTT) 27 seconds, Fibrinogen 300 mg/dL, D-Dimer 200 ng/mL.
Computed tomography (CT) of the abdomen and pelvis (Figure 1) was ordered which showed a thrombus within the inferior mesenteric vein (IMV) and the proximal branch of the right portal vein. Vascular surgery was consulted in the ED to assess for any acute intervention. However, given the CT abdomen and pelvis report and the normal lactic acid level, no acute intervention was needed. The patient was then admitted to medicine for hypercoagulability workup. Patient denied any family history of blood clotting disorders. He was started on intramuscular Lovenox 70 mg injection twice daily. Gastroenterology was consulted and recommended to trend liver function test. Hematology was consulted and recommended ordering (anticardiolipin antibodies, lupus anticoagulant, anti-beta-2-GPI antibodies, Factor V Leiden, Prothrombin gene, Antithrombin III, Homocysteine, protein C, and protein S) that were all negative for abnormalities. The patient’s pain and labs improved over the next couple of days, and was discharged on apixaban 10 mg twice daily for 7 days followed by 5 mg twice daily.
Discussion: This case highlights the unusual occurrence of concurrent thrombosis in the inferior mesenteric vein (IMV) and portal vein (PVT), emphasizing the importance of maintaining a high level of suspicion for thromboses in uncommon locations when patients present with abdominal pain.
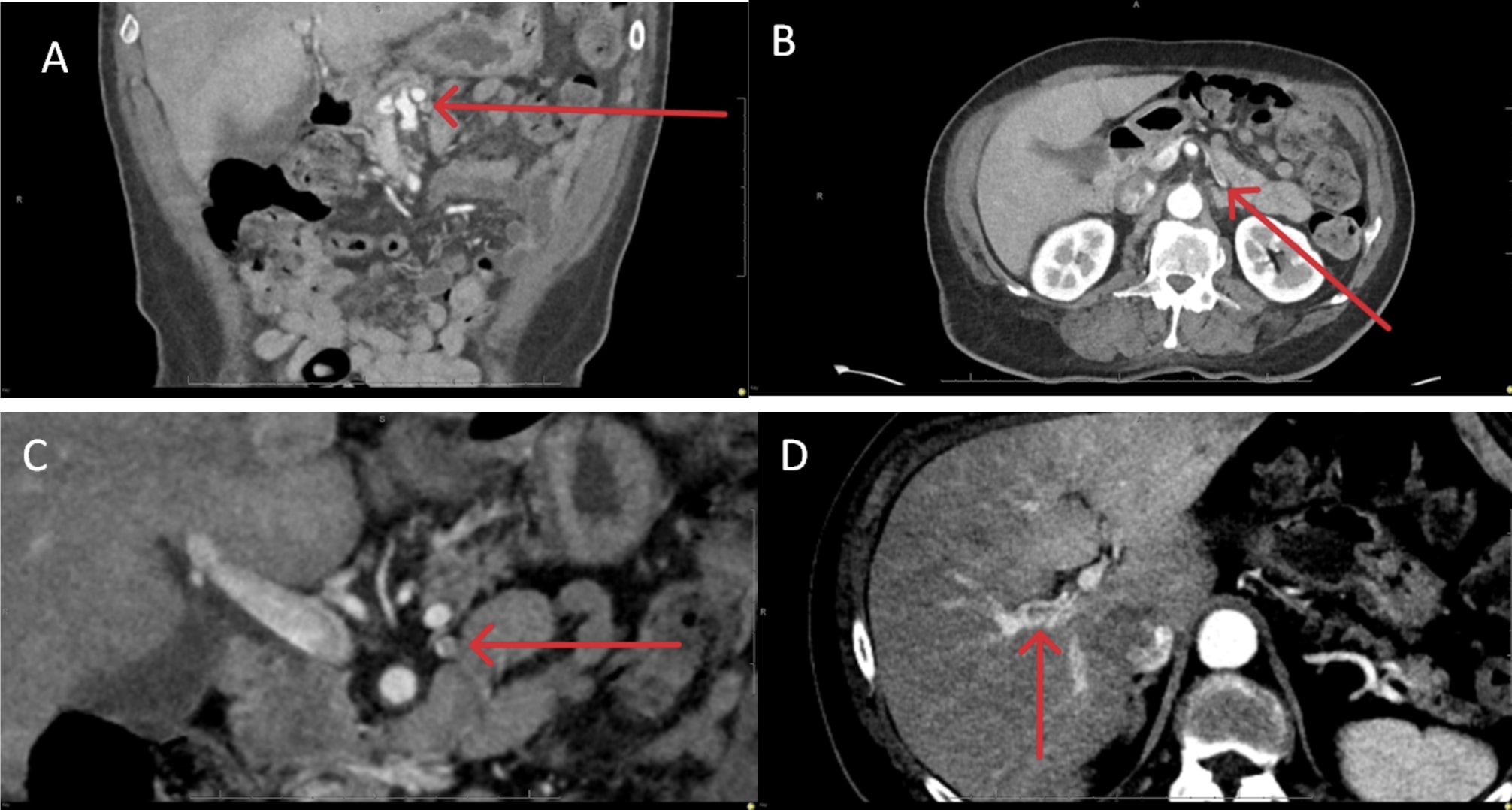
Figure: Figure 1: (A, B, C) Contrast Enhanced Computed Tomography (CT) scan of abdomen and pelvis showing filling defect within the inferior mesenteric vein consistent with non-occlusive thrombus. (D) filling defect within the right portal vein consistent with non-occlusive thrombus.
Disclosures:
Majd Khadra indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Rida Farook indicated no relevant financial relationships.
Camila Arellano indicated no relevant financial relationships.
Naveed Shaikh indicated no relevant financial relationships.
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Rida Farook, BS2, Camila Arellano, BS2, Naveed Shaikh, MD3. P1281 - Unveiling the Mystery of Veins: A Unique Combination of Portal and Inferior Mesenteric Venous Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
