Sunday Poster Session
Category: Liver
P1290 - Alcohol-Associated Hepatitis and Concurrent Non-Immune Hemolytic Anemia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NO
Nazli Begum Ozturk, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD1, Morgan Kiryakoza, MD2, Leandro Sierra, MD3, Justin K. Skrzynski, MD2
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Zieve’s syndrome describes a triad of non-immune hemolytic anemia, jaundice, and transient hyperlipidemia found in patients with alcohol-use disorder/alcohol-associated liver disease. This case involves a patient with suspected Zieve’s syndrome in the setting of severe alcohol-associated hepatitis.
Case Description/Methods: A 39-year-old female with alcohol-use disorder presented to the hospital with complaints of jaundice, lethargy, and confusion. On presentation, patient was anemic with a hemoglobin of 7.8 g/dL (12.1-15.0 g/dL), had ALP of 235 U/L (33-120 U/L), AST of 116 U/L (< 35 U/L), ALT of 41 (< 37 U/L) total bilirubin of 24.2 mg/dL (< 1.2mg/dL), direct bilirubin of >15 mg/dL (< 0.4 mg/dL). She was admitted due to concerns for alcohol-associated hepatitis. Her hospital course was complicated by frequent declines in hemoglobin requiring a total of six transfusions of packed red blood cells. No overt bleeding such as hematemesis or hematochezia was evident during these declines. Further hematologic workup revealed a normal glucose 6 phosphate dehydrogenase (G6PD), normal pyruvate kinase, elevated plasma hemoglobin of 150 mg/dL (< 30 mg/dL), decreased haptoglobin of < 8 mg/dL (40-250 mg/dL), elevated lactate dehydrogenase of 595 (100-240 U/L), and elevated reticulocyte count of 213 bil/L (21-100 bil/L). Direct Coombs Test was negative. The combination of these labs illustrated a picture of non-immune hemolytic anemia. Patient’s hospitalization was further complicated by the development of ascites and spontaneous bacterial peritonitis (SBP). Given the presence of SBP, corticosteroid therapy was not initiated for alcohol-associated hepatitis. Lipid panel remained within normal limits on two separate occasions. Vitamin E level was < 2.5 mg/L (5.5 – 17.0 mg/L). The patient was eventually discharged home with hospice and her hemoglobin levels remained stable after supportive blood transfusions during her stay.
Discussion: Zieve’s syndrome is an underdiagnosed cause of anemia in patients with alcohol-associated liver disease. There are multiple proposed mechanisms to explain the pathophysiology behind the red cell lysis seen in this disorder. One leading hypothesis suggests the red cell membrane becomes unstable due to vitamin E deficiency leading to disordered pyruvate kinase. Importance of early recognition of this syndrome is essential as treatment revolves around strict abstinence from alcohol.
Disclosures:
Nazli Begum Ozturk, MD1, Morgan Kiryakoza, MD2, Leandro Sierra, MD3, Justin K. Skrzynski, MD2. P1290 - Alcohol-Associated Hepatitis and Concurrent Non-Immune Hemolytic Anemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Zieve’s syndrome describes a triad of non-immune hemolytic anemia, jaundice, and transient hyperlipidemia found in patients with alcohol-use disorder/alcohol-associated liver disease. This case involves a patient with suspected Zieve’s syndrome in the setting of severe alcohol-associated hepatitis.
Case Description/Methods: A 39-year-old female with alcohol-use disorder presented to the hospital with complaints of jaundice, lethargy, and confusion. On presentation, patient was anemic with a hemoglobin of 7.8 g/dL (12.1-15.0 g/dL), had ALP of 235 U/L (33-120 U/L), AST of 116 U/L (< 35 U/L), ALT of 41 (< 37 U/L) total bilirubin of 24.2 mg/dL (< 1.2mg/dL), direct bilirubin of >15 mg/dL (< 0.4 mg/dL). She was admitted due to concerns for alcohol-associated hepatitis. Her hospital course was complicated by frequent declines in hemoglobin requiring a total of six transfusions of packed red blood cells. No overt bleeding such as hematemesis or hematochezia was evident during these declines. Further hematologic workup revealed a normal glucose 6 phosphate dehydrogenase (G6PD), normal pyruvate kinase, elevated plasma hemoglobin of 150 mg/dL (< 30 mg/dL), decreased haptoglobin of < 8 mg/dL (40-250 mg/dL), elevated lactate dehydrogenase of 595 (100-240 U/L), and elevated reticulocyte count of 213 bil/L (21-100 bil/L). Direct Coombs Test was negative. The combination of these labs illustrated a picture of non-immune hemolytic anemia. Patient’s hospitalization was further complicated by the development of ascites and spontaneous bacterial peritonitis (SBP). Given the presence of SBP, corticosteroid therapy was not initiated for alcohol-associated hepatitis. Lipid panel remained within normal limits on two separate occasions. Vitamin E level was < 2.5 mg/L (5.5 – 17.0 mg/L). The patient was eventually discharged home with hospice and her hemoglobin levels remained stable after supportive blood transfusions during her stay.
Discussion: Zieve’s syndrome is an underdiagnosed cause of anemia in patients with alcohol-associated liver disease. There are multiple proposed mechanisms to explain the pathophysiology behind the red cell lysis seen in this disorder. One leading hypothesis suggests the red cell membrane becomes unstable due to vitamin E deficiency leading to disordered pyruvate kinase. Importance of early recognition of this syndrome is essential as treatment revolves around strict abstinence from alcohol.
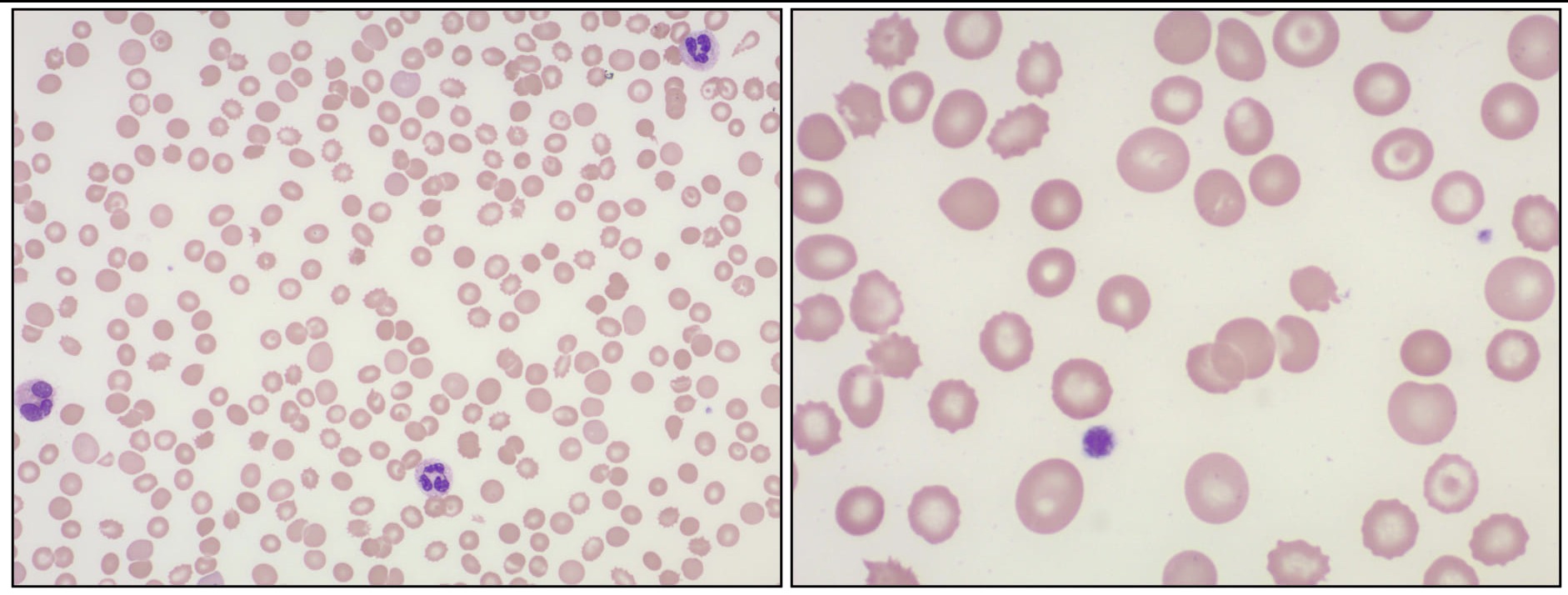
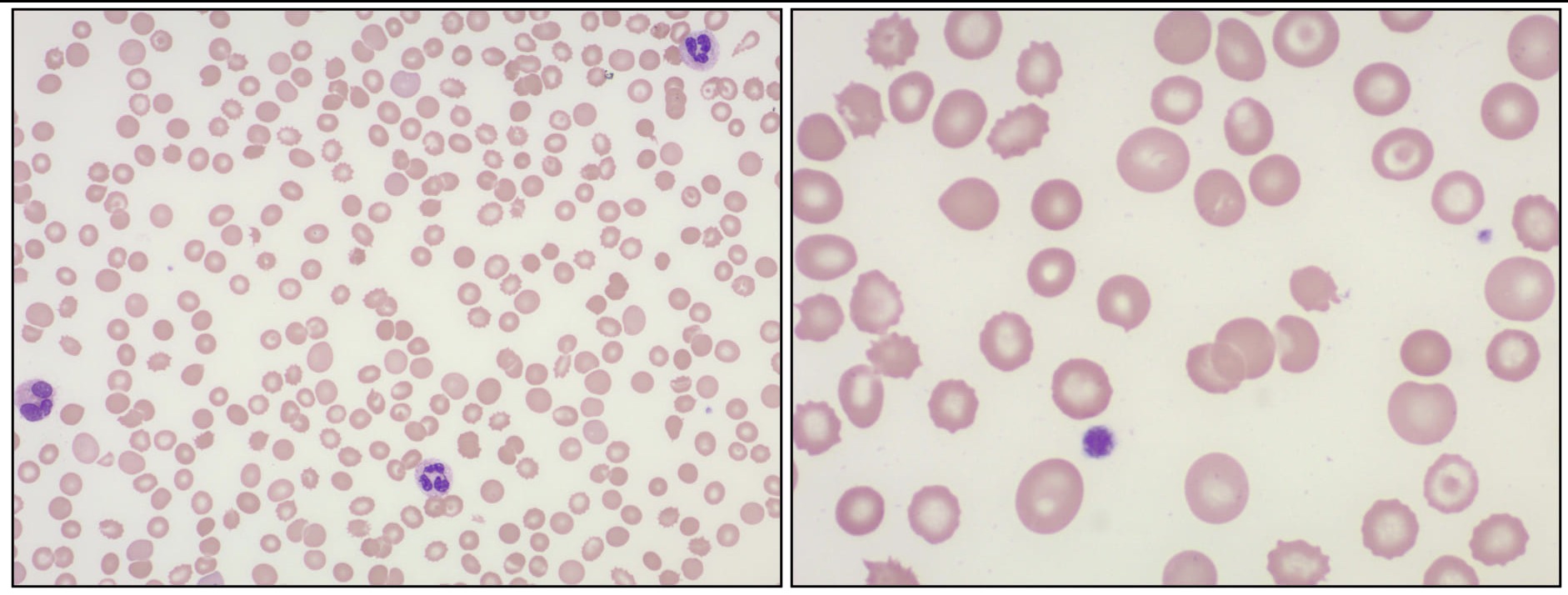
Figure: The red cells show mild anisopoikilocytosis with a few echinocytes, occasional spherocytes, acanthocytes or schistocytes.
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Morgan Kiryakoza indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Justin Skrzynski indicated no relevant financial relationships.
Nazli Begum Ozturk, MD1, Morgan Kiryakoza, MD2, Leandro Sierra, MD3, Justin K. Skrzynski, MD2. P1290 - Alcohol-Associated Hepatitis and Concurrent Non-Immune Hemolytic Anemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
