Sunday Poster Session
Category: Liver
P1295 - Hepatic Sarcoidosis Presenting With Abdominal Pain: A Comparison of a Rare Extrahepatic Disease Manifestation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rahul Sandella, MD
University of Chicago Medicine
Chicago, IL
Presenting Author(s)
Rahul Sandella, MD, Hannah Roth, MD, Sonali Paul, MD, MSc, Natali Ronen, MD, John Hart, MD, Alan L. Hutchison, MD, PhD
University of Chicago Medicine, Chicago, IL
Introduction: Hepatic sarcoidosis is a granulomatous disease affecting multiple organs. It is usually asymptomatic and often presents with elevated liver tests. Nonspecific symptoms including fatigue, pruritus, and hepatomegaly are sometimes seen. Here we discuss two cases of hepatic sarcoidosis that presented with rare extra-hepatic complications.
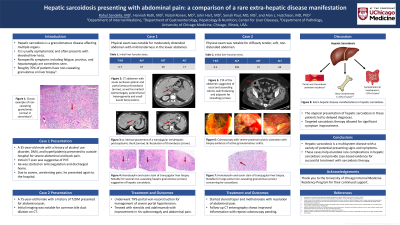
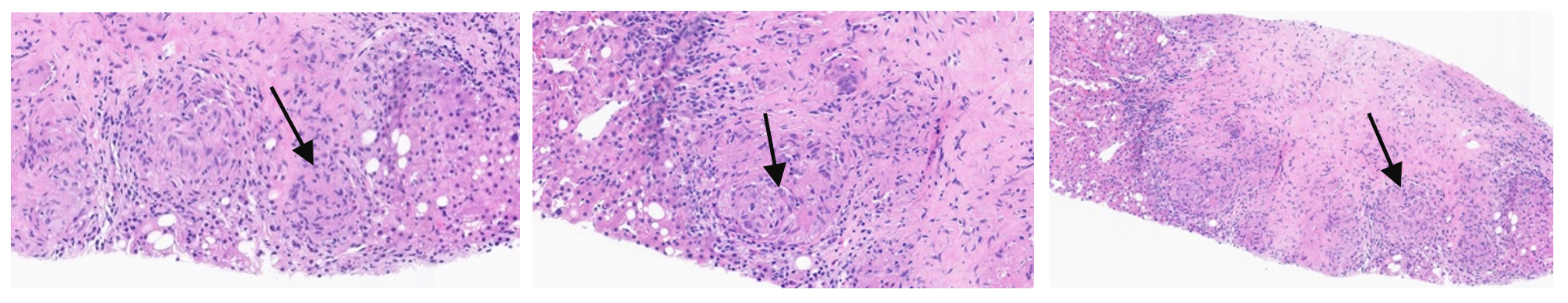
Case Description/Methods: Case 1: A 35-year-old male with history of alcohol use disorder presented with abdominal pain and was found to have extensive thrombus, involving the portal(PVT), splenic and superior mesenteric vein. CT also revealed bony lesions suggestive of a marrow infiltrative process concerning for malignancy. His liver tests were normal. Liver and bone marrow biopsies revealed granulomas concerning for sarcoidosis. He underwent transjugular intrahepatic portosystemic shunt to manage his PVT. He was then started on steroids and weekly adalimumab with resolution of symptoms and bone lesions.
Case 2: A 75-year-old woman presented with abdominal pain and new transaminitis. CT Imaging showed severe proximal colonic thickening with biopsies suggestive of active granulomatous colitis. Transaminitis continued to worsen so she underwent liver biopsies which were concerning for sarcoidosis. Colonic inflammation was deemed sequela of sarcoidosis with abdominal pain improvement and resolution of colonic thickening following steroid therapy.
Discussion: In the first case, the presence of extensive clot, lymphadenopathy, and lytic bone lesions was initially concerning for malignancy; it was not until both bone marrow and liver biopsies revealed granulomas that a diagnosis of sarcoidosis could confidently be made. The incidence of PVT in hepatic sarcoidosis is not well reported but is likely a sequela of portal hypertension. Bony involvement has also been reported in around 1-15% of hepatic sarcoidosis cases. In the second case, presence of proximal colonic inflammation led initially to a presumed diagnosis of inflammatory bowel disease. Biopsy confirmed hepatic sarcoidosis, which can be associated with symptomatic GI involvement in < 1% of cases. Although these patients had delayed diagnoses due to the need to rule out more common diseases, both had symptom improvement following sarcoidosis therapy. Hepatic sarcoidosis is a multisystem disease with a variety of potential presenting signs and symptoms. These cases help elucidate rare complications in hepatic sarcoidosis and provide case-based evidence for successful treatment with steroid therapy.
Disclosures:
Rahul Sandella, MD, Hannah Roth, MD, Sonali Paul, MD, MSc, Natali Ronen, MD, John Hart, MD, Alan L. Hutchison, MD, PhD. P1295 - Hepatic Sarcoidosis Presenting With Abdominal Pain: A Comparison of a Rare Extrahepatic Disease Manifestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Chicago Medicine, Chicago, IL
Introduction: Hepatic sarcoidosis is a granulomatous disease affecting multiple organs. It is usually asymptomatic and often presents with elevated liver tests. Nonspecific symptoms including fatigue, pruritus, and hepatomegaly are sometimes seen. Here we discuss two cases of hepatic sarcoidosis that presented with rare extra-hepatic complications.
Case Description/Methods: Case 1: A 35-year-old male with history of alcohol use disorder presented with abdominal pain and was found to have extensive thrombus, involving the portal(PVT), splenic and superior mesenteric vein. CT also revealed bony lesions suggestive of a marrow infiltrative process concerning for malignancy. His liver tests were normal. Liver and bone marrow biopsies revealed granulomas concerning for sarcoidosis. He underwent transjugular intrahepatic portosystemic shunt to manage his PVT. He was then started on steroids and weekly adalimumab with resolution of symptoms and bone lesions.
Case 2: A 75-year-old woman presented with abdominal pain and new transaminitis. CT Imaging showed severe proximal colonic thickening with biopsies suggestive of active granulomatous colitis. Transaminitis continued to worsen so she underwent liver biopsies which were concerning for sarcoidosis. Colonic inflammation was deemed sequela of sarcoidosis with abdominal pain improvement and resolution of colonic thickening following steroid therapy.
Discussion: In the first case, the presence of extensive clot, lymphadenopathy, and lytic bone lesions was initially concerning for malignancy; it was not until both bone marrow and liver biopsies revealed granulomas that a diagnosis of sarcoidosis could confidently be made. The incidence of PVT in hepatic sarcoidosis is not well reported but is likely a sequela of portal hypertension. Bony involvement has also been reported in around 1-15% of hepatic sarcoidosis cases. In the second case, presence of proximal colonic inflammation led initially to a presumed diagnosis of inflammatory bowel disease. Biopsy confirmed hepatic sarcoidosis, which can be associated with symptomatic GI involvement in < 1% of cases. Although these patients had delayed diagnoses due to the need to rule out more common diseases, both had symptom improvement following sarcoidosis therapy. Hepatic sarcoidosis is a multisystem disease with a variety of potential presenting signs and symptoms. These cases help elucidate rare complications in hepatic sarcoidosis and provide case-based evidence for successful treatment with steroid therapy.
Figure: Figure 1: Hematoxylin and eosin stain of transjugular liver biopsy from the 35-year-old male in case 1. Notable for several non-caseating hepatic granulomas (representative examples marked by arrows) suggestive of hepatic sarcoidosis.
Disclosures:
Rahul Sandella indicated no relevant financial relationships.
Hannah Roth indicated no relevant financial relationships.
Sonali Paul: Intercept – Grant/Research Support. TARGET PharmaSolutions – Grant/Research Support.
Natali Ronen indicated no relevant financial relationships.
John Hart indicated no relevant financial relationships.
Alan Hutchison indicated no relevant financial relationships.
Rahul Sandella, MD, Hannah Roth, MD, Sonali Paul, MD, MSc, Natali Ronen, MD, John Hart, MD, Alan L. Hutchison, MD, PhD. P1295 - Hepatic Sarcoidosis Presenting With Abdominal Pain: A Comparison of a Rare Extrahepatic Disease Manifestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
