Sunday Poster Session
Category: Liver
P1211 - The Catch Up: Improving Hepatitis B Screening and Vaccination Rates Among High-Risk Ethnic Minorities
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Makeda Dawkins, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Award: Presidential Poster Award
Makeda Dawkins, MD1, Alexander Levstik, MBBS1, Nicholas Cheung, BS2, Gabriel Heering, MD1, Melissa Gennarelli, MD1, Jason Goutis, MD1, Christopher Nabors, MD, PhD1, David C.. Wolf, MD, FACG1
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
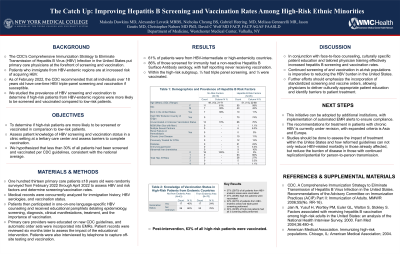
Introduction: The CDC's Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus (HBV) Infection in the United States put primary care physicians at the forefront of screening and vaccination. Patients who immigrate from HBV-endemic regions are at increased risk of acquiring HBV. As of February 2022, the CDC recommends that all individuals over 18 years old have one-time HBV triple-panel screening and vaccination if susceptible. We studied the prevalence of HBV screening and vaccination to determine if high-risk patients from HBV-endemic regions were more likely to be screened and vaccinated compared to low-risk patients.
Methods: One hundred thirteen primary care patients ≥18 years old were randomly surveyed from February 2022 through April 2022 to assess HBV and risk factors and determine screening/vaccination rates. Medical records were analyzed for immigration history, HBV serologies, and vaccination status. We hypothesized that less than 30% of all patients had been screened and vaccinated per CDC guidelines, consistent with the national average. Patients then participated in one-on-one language-specific HBV counseling and received educational pamphlets detailing epidemiology, screening, diagnosis, clinical manifestations, treatment, and the importance of vaccination. Primary care providers were educated on new CDC guidelines, and automatic order sets were incorporated into EMRs. Patient records were reviewed six months later to assess the impact of the educational intervention. Patients were also interviewed by telephone to capture off-site testing and vaccination.
Results: 61% of patients were from HBV-intermediate or high-endemicity countries. 86% of those screened for immunity had a non-reactive Hepatitis B Surface Antibody serology, with half reporting never receiving vaccination. Within the high-risk subgroup, ⅓ had triple panel screening, and ⅓ were vaccinated. Post-intervention, 63% of all high-risk patients were vaccinated.
Discussion: In conjunction with face-to-face counseling, culturally specific patient education and tailored physician training effectively increased hepatitis B screening and vaccination rates. Continued screening of and vaccination in at-risk populations is imperative to reducing the HBV burden in the United States. Further efforts should emphasize the incorporation of standardized screening and vaccine orders, allowing physicians to deliver culturally appropriate patient education and identify barriers to patient treatment.
Disclosures:
Makeda Dawkins, MD1, Alexander Levstik, MBBS1, Nicholas Cheung, BS2, Gabriel Heering, MD1, Melissa Gennarelli, MD1, Jason Goutis, MD1, Christopher Nabors, MD, PhD1, David C.. Wolf, MD, FACG1. P1211 - The Catch Up: Improving Hepatitis B Screening and Vaccination Rates Among High-Risk Ethnic Minorities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Makeda Dawkins, MD1, Alexander Levstik, MBBS1, Nicholas Cheung, BS2, Gabriel Heering, MD1, Melissa Gennarelli, MD1, Jason Goutis, MD1, Christopher Nabors, MD, PhD1, David C.. Wolf, MD, FACG1
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
Introduction: The CDC's Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus (HBV) Infection in the United States put primary care physicians at the forefront of screening and vaccination. Patients who immigrate from HBV-endemic regions are at increased risk of acquiring HBV. As of February 2022, the CDC recommends that all individuals over 18 years old have one-time HBV triple-panel screening and vaccination if susceptible. We studied the prevalence of HBV screening and vaccination to determine if high-risk patients from HBV-endemic regions were more likely to be screened and vaccinated compared to low-risk patients.
Methods: One hundred thirteen primary care patients ≥18 years old were randomly surveyed from February 2022 through April 2022 to assess HBV and risk factors and determine screening/vaccination rates. Medical records were analyzed for immigration history, HBV serologies, and vaccination status. We hypothesized that less than 30% of all patients had been screened and vaccinated per CDC guidelines, consistent with the national average. Patients then participated in one-on-one language-specific HBV counseling and received educational pamphlets detailing epidemiology, screening, diagnosis, clinical manifestations, treatment, and the importance of vaccination. Primary care providers were educated on new CDC guidelines, and automatic order sets were incorporated into EMRs. Patient records were reviewed six months later to assess the impact of the educational intervention. Patients were also interviewed by telephone to capture off-site testing and vaccination.
Results: 61% of patients were from HBV-intermediate or high-endemicity countries. 86% of those screened for immunity had a non-reactive Hepatitis B Surface Antibody serology, with half reporting never receiving vaccination. Within the high-risk subgroup, ⅓ had triple panel screening, and ⅓ were vaccinated. Post-intervention, 63% of all high-risk patients were vaccinated.
Discussion: In conjunction with face-to-face counseling, culturally specific patient education and tailored physician training effectively increased hepatitis B screening and vaccination rates. Continued screening of and vaccination in at-risk populations is imperative to reducing the HBV burden in the United States. Further efforts should emphasize the incorporation of standardized screening and vaccine orders, allowing physicians to deliver culturally appropriate patient education and identify barriers to patient treatment.
Disclosures:
Makeda Dawkins indicated no relevant financial relationships.
Alexander Levstik indicated no relevant financial relationships.
Nicholas Cheung indicated no relevant financial relationships.
Gabriel Heering indicated no relevant financial relationships.
Melissa Gennarelli indicated no relevant financial relationships.
Jason Goutis indicated no relevant financial relationships.
Christopher Nabors indicated no relevant financial relationships.
David Wolf indicated no relevant financial relationships.
Makeda Dawkins, MD1, Alexander Levstik, MBBS1, Nicholas Cheung, BS2, Gabriel Heering, MD1, Melissa Gennarelli, MD1, Jason Goutis, MD1, Christopher Nabors, MD, PhD1, David C.. Wolf, MD, FACG1. P1211 - The Catch Up: Improving Hepatitis B Screening and Vaccination Rates Among High-Risk Ethnic Minorities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

