Sunday Poster Session
Category: Liver
P1144 - Disparities in the Decision to Evaluate for Liver Transplant in Patients Referred With Underlying Alcohol-Associated Liver Disease (ALD)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RO
Rafael Ornelas, MD
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Award: ACG Outstanding Research Award in the Liver Category (Trainee)
Award: Presidential Poster Award
Rafael Ornelas, MD, Julia Hamilton, MD, Ellen Clark, MD, Scott Naugler, MD
Oregon Health & Science University, Portland, OR
Introduction: Alcohol associated liver disease (ALD) has been the leading indication for liver transplantation (LT) in the United States since surpassing HCV in 2016. Patients transplanted for ALD generally do well but are a highly selected group of patients from a large pool of patients with Alcohol Use Disorder (AUD) and ALD. We are still learning which patients from this pool benefit the most from LT, and many cultural biases inform decisions about offering LT to patients with ALD. Little data on the earliest phases of the LT process (referral and triage) are available on these important decisions to offer LT to this vulnerable group of patients. We hypothesize that patients with ALD referred for LT may be evaluated at lower rates than patients with other etiologies of liver disease.
Methods: This is a single center, retrospective cohort study including patients referred for LT between 2018 and 2022. Patients with a MELD score of > 15 or hepatocellular carcinoma (HCC) were included in the study. Data collected included patient demographics, liver disease diagnosis, and the time of referral, evaluation, listing and time of liver transplant. Reason(s) for the removal or decline of the patient at any juncture within the liver transplant process were collected and categorized after review.
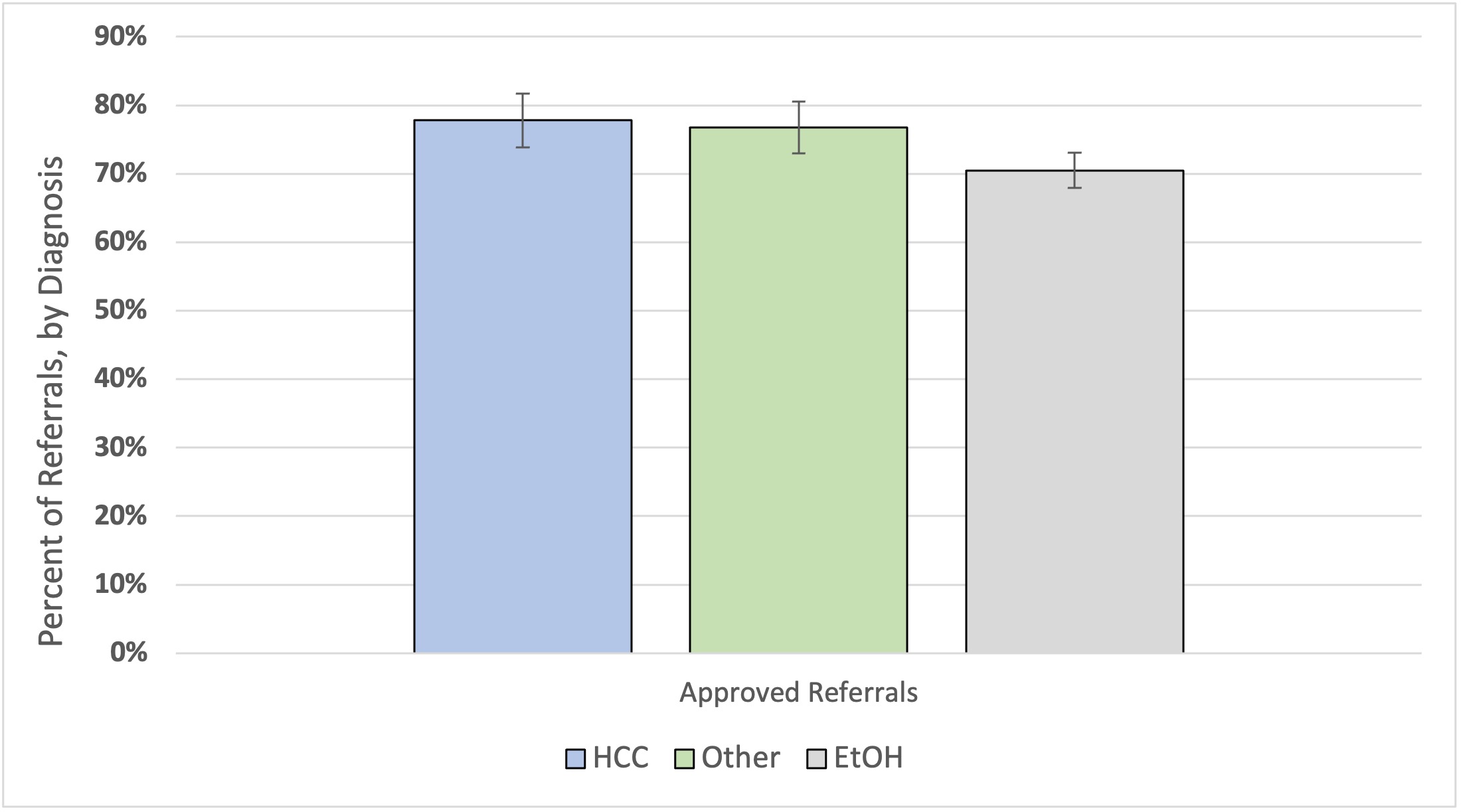
Results: Between 2018 and 2022, 704 referrals for liver transplantation were reviewed and screened of which 610 met inclusion criteria. Of those patients referred, 52% had a primary or secondary diagnosis of ALD, 22.3% had underlying HCC, and 26.7% with other liver disease (non-ALD and non-HCC disease). 70 % of referrals in those with ALD were accepted for evaluation compared to 77% of other diseases and 78% of those with HCC (p = 0.20). Compared to patients in other groups, those with ALD were significantly more likely to be perceived high risk to harmful drinking (p = < 0.001) by the reviewing physician.
Discussion: Patients with ALD were denied more LT evaluations compared to patients to non-ALD, although this outcome did not reach statistical significance. However, the reasons for denying a LT evaluation in those with ALD was driven in part by cultural perceptions of patients with ALD, rather than an assessment of whether the patients would benefit from LT based on the available outcome data.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rafael Ornelas, MD, Julia Hamilton, MD, Ellen Clark, MD, Scott Naugler, MD. P1144 - Disparities in the Decision to Evaluate for Liver Transplant in Patients Referred With Underlying Alcohol-Associated Liver Disease (ALD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Award: Presidential Poster Award
Rafael Ornelas, MD, Julia Hamilton, MD, Ellen Clark, MD, Scott Naugler, MD
Oregon Health & Science University, Portland, OR
Introduction: Alcohol associated liver disease (ALD) has been the leading indication for liver transplantation (LT) in the United States since surpassing HCV in 2016. Patients transplanted for ALD generally do well but are a highly selected group of patients from a large pool of patients with Alcohol Use Disorder (AUD) and ALD. We are still learning which patients from this pool benefit the most from LT, and many cultural biases inform decisions about offering LT to patients with ALD. Little data on the earliest phases of the LT process (referral and triage) are available on these important decisions to offer LT to this vulnerable group of patients. We hypothesize that patients with ALD referred for LT may be evaluated at lower rates than patients with other etiologies of liver disease.
Methods: This is a single center, retrospective cohort study including patients referred for LT between 2018 and 2022. Patients with a MELD score of > 15 or hepatocellular carcinoma (HCC) were included in the study. Data collected included patient demographics, liver disease diagnosis, and the time of referral, evaluation, listing and time of liver transplant. Reason(s) for the removal or decline of the patient at any juncture within the liver transplant process were collected and categorized after review.
Results: Between 2018 and 2022, 704 referrals for liver transplantation were reviewed and screened of which 610 met inclusion criteria. Of those patients referred, 52% had a primary or secondary diagnosis of ALD, 22.3% had underlying HCC, and 26.7% with other liver disease (non-ALD and non-HCC disease). 70 % of referrals in those with ALD were accepted for evaluation compared to 77% of other diseases and 78% of those with HCC (p = 0.20). Compared to patients in other groups, those with ALD were significantly more likely to be perceived high risk to harmful drinking (p = < 0.001) by the reviewing physician.
Discussion: Patients with ALD were denied more LT evaluations compared to patients to non-ALD, although this outcome did not reach statistical significance. However, the reasons for denying a LT evaluation in those with ALD was driven in part by cultural perceptions of patients with ALD, rather than an assessment of whether the patients would benefit from LT based on the available outcome data.
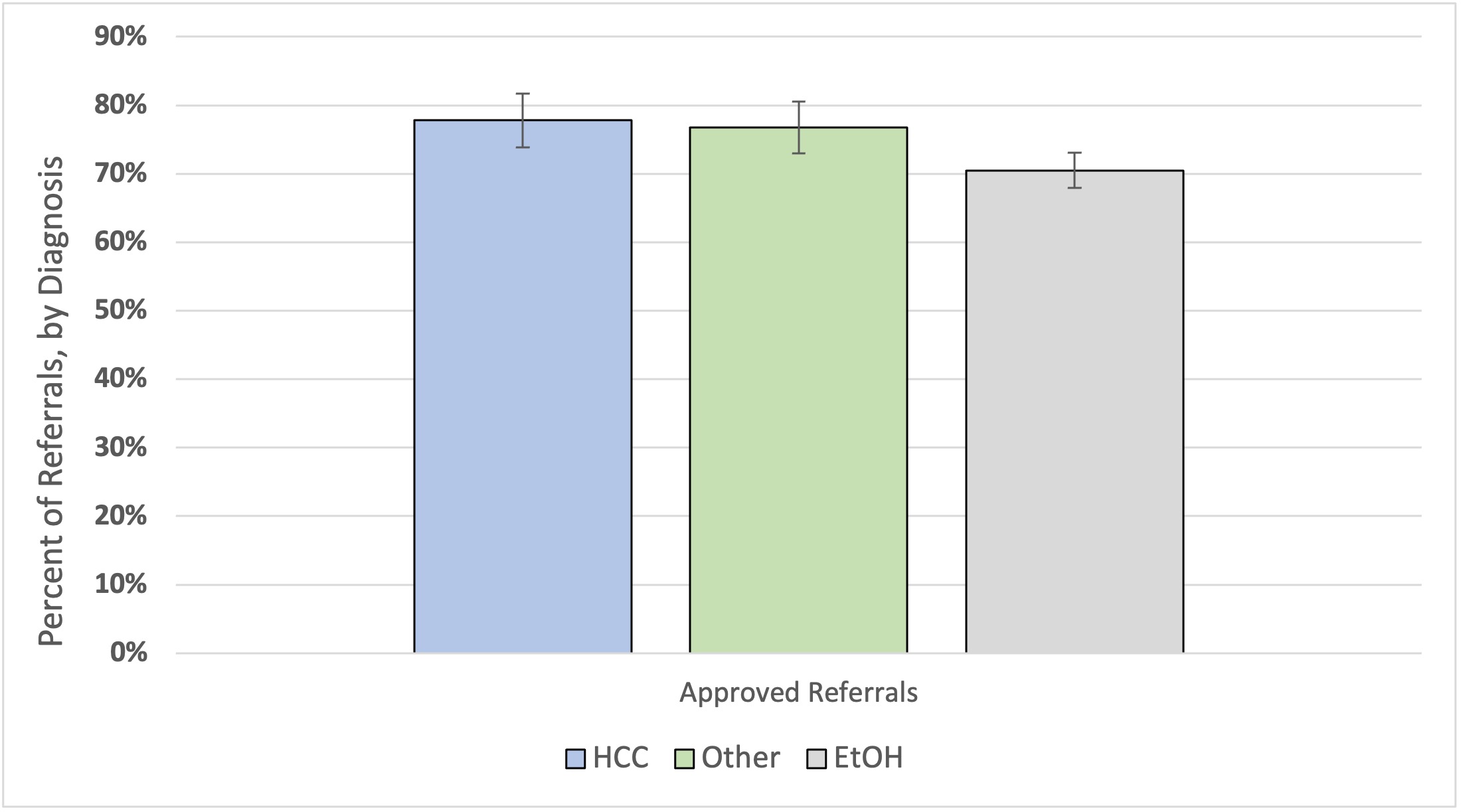
Figure: Percent of Liver Transplant Referrals Approved
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rafael Ornelas indicated no relevant financial relationships.
Julia Hamilton indicated no relevant financial relationships.
Ellen Clark indicated no relevant financial relationships.
Scott Naugler indicated no relevant financial relationships.
Rafael Ornelas, MD, Julia Hamilton, MD, Ellen Clark, MD, Scott Naugler, MD. P1144 - Disparities in the Decision to Evaluate for Liver Transplant in Patients Referred With Underlying Alcohol-Associated Liver Disease (ALD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

