Sunday Poster Session
Category: Liver
P1154 - Hepatology Management of Adults with Fontan Circulation: An Interdisciplinary Protocol
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suhaib Alhaj Ali, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Suhib Alhaj Ali, MD1, Sanad Dawod, MD2, Ahmad Alomari, MD1, Haya Omeish, MD2, Kevin Cobty, BS3, Omar Shamaa, MD2, Shannon Todd, MHS1, Celeste Williams, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI
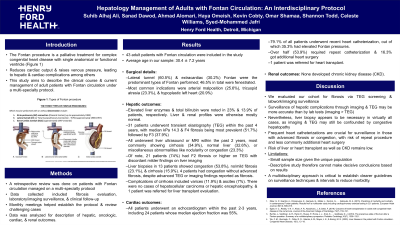
Introduction: The Fontan procedure is a palliative treatment for complex congenital heart disease that reduces cardiac output & raises venous pressure, leading to hepatic & cardiac complications. This study describes the clinical course & current management of adult patients with Fontan circulation under an interdisciplinary protocol.
Methods: A retrospective review was done on adult patients with Fontan circulation after data collection on fibrosis evaluation, laboratory/imaging surveillance, & clinical follow-up. Monthly meetings helped establish the protocol & review challenging cases. Data was analyzed for describing hepatic, oncologic, cardiac, & renal outcomes.
Results: 43 patients were included, average age 30.4 ± 7.2 years. Lateral tunnel (60.5%) & extracardiac (30.2%) Fontan were predominant; 46.5% were fenestrated. Indications included arterial malposition (25.6%), tricuspid atresia (23.3%), & hypoplastic left heart (20.9%). Elevated liver enzymes & total bilirubin were noted in 23% & 13.9%, respectively. Transient elastography (TEG) was done on 31 patients showing median stiffness of 14.3 kPa, with 51.7% having F4 fibrosis & 37.9% F3. All patients underwent liver US or MRI within the last 2 years, revealing cirrhosis in 34.9% & congestion in 23.3%. Despite lacking imaging evidence of fibrosis, 21 had F2 or higher fibrosis on TEG. Liver biopsies in 13 patients showed congestion (53.8%), no/mild fibrosis (23.1%), & cirrhosis (15.9%). 4 patients had congestion without advanced fibrosis, despite advanced TEG or imaging findings. Cirrhotic complications included varices (11.9%) & ascites (7%). There were no cases of hepatocellular carcinoma or hepatic encephalopathy, & 1 patient was referred for liver transplant evaluation. Median ejection fraction was 55%. Heart catheterizations were done in 79.1%, 35.3% of whom had high Fontan pressures. Over half (53.9%) required repeat catheterization & 16.3% got additional heart surgery. 1 patient was referred for heart transplant. None developed chronic kidney disease (CKD).
Discussion: Our results show that fibrosis evaluation via TEG screening & laboratory/imaging surveillance may be confounded by congestive hepatopathy, commonly necessitating liver biopsy. Frequent heart catheterizations are crucial for surveillance in those with advanced fibrosis or congestion. Risk of liver or heart transplant as well as CKD remains low. An interdisciplinary protocol is imperative to establish clearer guidelines on surveillance techniques/intervals to reduce morbidity.
Disclosures:
Suhib Alhaj Ali, MD1, Sanad Dawod, MD2, Ahmad Alomari, MD1, Haya Omeish, MD2, Kevin Cobty, BS3, Omar Shamaa, MD2, Shannon Todd, MHS1, Celeste Williams, MD1, Syed-Mohammed Jafri, MD2. P1154 - Hepatology Management of Adults with Fontan Circulation: An Interdisciplinary Protocol, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI
Introduction: The Fontan procedure is a palliative treatment for complex congenital heart disease that reduces cardiac output & raises venous pressure, leading to hepatic & cardiac complications. This study describes the clinical course & current management of adult patients with Fontan circulation under an interdisciplinary protocol.
Methods: A retrospective review was done on adult patients with Fontan circulation after data collection on fibrosis evaluation, laboratory/imaging surveillance, & clinical follow-up. Monthly meetings helped establish the protocol & review challenging cases. Data was analyzed for describing hepatic, oncologic, cardiac, & renal outcomes.
Results: 43 patients were included, average age 30.4 ± 7.2 years. Lateral tunnel (60.5%) & extracardiac (30.2%) Fontan were predominant; 46.5% were fenestrated. Indications included arterial malposition (25.6%), tricuspid atresia (23.3%), & hypoplastic left heart (20.9%). Elevated liver enzymes & total bilirubin were noted in 23% & 13.9%, respectively. Transient elastography (TEG) was done on 31 patients showing median stiffness of 14.3 kPa, with 51.7% having F4 fibrosis & 37.9% F3. All patients underwent liver US or MRI within the last 2 years, revealing cirrhosis in 34.9% & congestion in 23.3%. Despite lacking imaging evidence of fibrosis, 21 had F2 or higher fibrosis on TEG. Liver biopsies in 13 patients showed congestion (53.8%), no/mild fibrosis (23.1%), & cirrhosis (15.9%). 4 patients had congestion without advanced fibrosis, despite advanced TEG or imaging findings. Cirrhotic complications included varices (11.9%) & ascites (7%). There were no cases of hepatocellular carcinoma or hepatic encephalopathy, & 1 patient was referred for liver transplant evaluation. Median ejection fraction was 55%. Heart catheterizations were done in 79.1%, 35.3% of whom had high Fontan pressures. Over half (53.9%) required repeat catheterization & 16.3% got additional heart surgery. 1 patient was referred for heart transplant. None developed chronic kidney disease (CKD).
Discussion: Our results show that fibrosis evaluation via TEG screening & laboratory/imaging surveillance may be confounded by congestive hepatopathy, commonly necessitating liver biopsy. Frequent heart catheterizations are crucial for surveillance in those with advanced fibrosis or congestion. Risk of liver or heart transplant as well as CKD remains low. An interdisciplinary protocol is imperative to establish clearer guidelines on surveillance techniques/intervals to reduce morbidity.
Disclosures:
Suhib Alhaj Ali indicated no relevant financial relationships.
Sanad Dawod indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Haya Omeish indicated no relevant financial relationships.
Kevin Cobty indicated no relevant financial relationships.
Omar Shamaa indicated no relevant financial relationships.
Shannon Todd indicated no relevant financial relationships.
Celeste Williams indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie, Intercept, VectivBio – Advisor or Review Panel Member, Speakers Bureau.
Suhib Alhaj Ali, MD1, Sanad Dawod, MD2, Ahmad Alomari, MD1, Haya Omeish, MD2, Kevin Cobty, BS3, Omar Shamaa, MD2, Shannon Todd, MHS1, Celeste Williams, MD1, Syed-Mohammed Jafri, MD2. P1154 - Hepatology Management of Adults with Fontan Circulation: An Interdisciplinary Protocol, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
