Sunday Poster Session
Category: Interventional Endoscopy
P1068 - Efficacy and Safety of Endoscopic Ultrasound-Guided Biliary Drainage in Malignant Hilar Obstruction: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RK
Rahul Karna, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Rahul Karna, MD1, Amir Sultan Seid, MD2, Gaurav Suryawanshi, MD1, Tanisha Kalra, MD3, Parth Patel, MD4, Muhammad Ali Butt, MD5, Himsikhar Khataniar, MD5, Shifa Umar, MD6, Neil Nero, 7, Mohammad Bilal, MD8
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3SUNY Downstate Health Sciences University, New York, NY; 4Ascension Saint Joseph Hospital, Chicago, IL; 5Allegheny General Hospital, Pittsburgh, PA; 6Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 7Cleveland Clinic, Cleveland, OH; 8University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
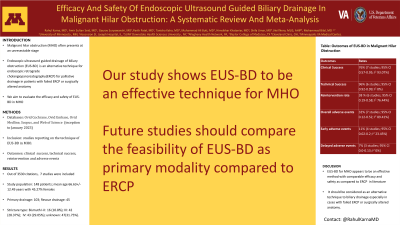
Introduction: Malignant hilar obstruction (MHO) often presents at an unresectable stage. Endoscopic ultrasound guided drainage of biliary obstruction (EUS-BD) is an alternative technique for endoscopic retrograde cholangiopancreatography(ERCP) for palliative drainage in patients with failed ERCP or surgically altered anatomy. We conducted this systematic review and meta-analysis to evaluate the efficacy and safety of EUS-BD in MHO.
Methods: We conducted a comprehensive search of Ovid Cochrane, Ovid Embase, Ovid Medline, Scopus, and Web of Science (inception to January 2023) to identify studies reporting on the technique of EUS-BD in MHO. The primary outcome was clinical success; secondary outcomes were technical success, reintervention and adverse events. A meta-analysis of proportions was done for all primary and secondary outcomes.
Results: Out of 3530 citations, a total of 7 studies were included. Study population consisted of 148 patients; mean age 66.63+/-12.49 years with 45.27% females. 103 patients underwent initial EUS-BD while 45 patients underwent rescue EUS-BD. Stricture type was Bismuth I-II: 16 (10.8%); Bismuth III: 42 (28.37%); Bismuth IV: 43 (29.05%); unknown: 47(31.75%). Etiology was gall bladder cancer: 16 (10.81%); Pancreatic cancer: 56 (37.83%); Cholangiocarcinoma 27 (18.24%); Others 49 (33.10%). Clinical success of EUS-BD in MHO was 76% (7 studies; 95% CI 0.57-0.95; I2 93.07%) while technical success was 96% (6 studies; 95% CI 0.92-0.99; I2 0%) . Reintervention rate was 38 % (6 studies; 95% CI 0.19-0.58; I2 76.44%). Overall adverse events were 32% (7 studies; 95% CI 0.12-0.52; I2 89.41%). Early adverse events were 11% (4 studies; 95% CI 0.02-0.2; I2 23.45%) while delayed adverse events were 7% (3 studies; 95% CI 0.0-0.13; I2 0%).
Discussion: EUS-BD for MHO appears to be an effective method with comparable efficacy and safety as compared to ERCP in literature. It should be considered as an alternative technique to biliary drainage especially in cases with failed ERCP or surgically altered anatomy. Future studies should be designed to compare its feasibility as a primary modality as compared to traditional methods like ERCP and percutaneous biliary drainage.
Disclosures:
Rahul Karna, MD1, Amir Sultan Seid, MD2, Gaurav Suryawanshi, MD1, Tanisha Kalra, MD3, Parth Patel, MD4, Muhammad Ali Butt, MD5, Himsikhar Khataniar, MD5, Shifa Umar, MD6, Neil Nero, 7, Mohammad Bilal, MD8. P1068 - Efficacy and Safety of Endoscopic Ultrasound-Guided Biliary Drainage in Malignant Hilar Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3SUNY Downstate Health Sciences University, New York, NY; 4Ascension Saint Joseph Hospital, Chicago, IL; 5Allegheny General Hospital, Pittsburgh, PA; 6Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 7Cleveland Clinic, Cleveland, OH; 8University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Malignant hilar obstruction (MHO) often presents at an unresectable stage. Endoscopic ultrasound guided drainage of biliary obstruction (EUS-BD) is an alternative technique for endoscopic retrograde cholangiopancreatography(ERCP) for palliative drainage in patients with failed ERCP or surgically altered anatomy. We conducted this systematic review and meta-analysis to evaluate the efficacy and safety of EUS-BD in MHO.
Methods: We conducted a comprehensive search of Ovid Cochrane, Ovid Embase, Ovid Medline, Scopus, and Web of Science (inception to January 2023) to identify studies reporting on the technique of EUS-BD in MHO. The primary outcome was clinical success; secondary outcomes were technical success, reintervention and adverse events. A meta-analysis of proportions was done for all primary and secondary outcomes.
Results: Out of 3530 citations, a total of 7 studies were included. Study population consisted of 148 patients; mean age 66.63+/-12.49 years with 45.27% females. 103 patients underwent initial EUS-BD while 45 patients underwent rescue EUS-BD. Stricture type was Bismuth I-II: 16 (10.8%); Bismuth III: 42 (28.37%); Bismuth IV: 43 (29.05%); unknown: 47(31.75%). Etiology was gall bladder cancer: 16 (10.81%); Pancreatic cancer: 56 (37.83%); Cholangiocarcinoma 27 (18.24%); Others 49 (33.10%). Clinical success of EUS-BD in MHO was 76% (7 studies; 95% CI 0.57-0.95; I2 93.07%) while technical success was 96% (6 studies; 95% CI 0.92-0.99; I2 0%) . Reintervention rate was 38 % (6 studies; 95% CI 0.19-0.58; I2 76.44%). Overall adverse events were 32% (7 studies; 95% CI 0.12-0.52; I2 89.41%). Early adverse events were 11% (4 studies; 95% CI 0.02-0.2; I2 23.45%) while delayed adverse events were 7% (3 studies; 95% CI 0.0-0.13; I2 0%).
Discussion: EUS-BD for MHO appears to be an effective method with comparable efficacy and safety as compared to ERCP in literature. It should be considered as an alternative technique to biliary drainage especially in cases with failed ERCP or surgically altered anatomy. Future studies should be designed to compare its feasibility as a primary modality as compared to traditional methods like ERCP and percutaneous biliary drainage.
Disclosures:
Rahul Karna indicated no relevant financial relationships.
Amir Sultan Seid indicated no relevant financial relationships.
Gaurav Suryawanshi indicated no relevant financial relationships.
Tanisha Kalra indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Muhammad Ali Butt indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Shifa Umar indicated no relevant financial relationships.
Neil Nero indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Rahul Karna, MD1, Amir Sultan Seid, MD2, Gaurav Suryawanshi, MD1, Tanisha Kalra, MD3, Parth Patel, MD4, Muhammad Ali Butt, MD5, Himsikhar Khataniar, MD5, Shifa Umar, MD6, Neil Nero, 7, Mohammad Bilal, MD8. P1068 - Efficacy and Safety of Endoscopic Ultrasound-Guided Biliary Drainage in Malignant Hilar Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
