Sunday Poster Session
Category: Interventional Endoscopy
P1071 - An Audit of Indications for Endoscopic Submucosal Dissection for Colorectal Lesions in North America: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Taylor Bowler, DO
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Taylor Bowler, DO1, Erica Loon, DO2, Sahib Singh, MD3, Himsikhar Khataniar, MD4, Muhammad Ali Butt, MD4, Nicole Theis-Mahon, 2, Rahul Karna, MD2, Natalie Wilson, MD2, Mohammad Bilal, MD5
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3Sinai Hospital, Baltimore, MD; 4Allegheny General Hospital, Pittsburgh, PA; 5University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
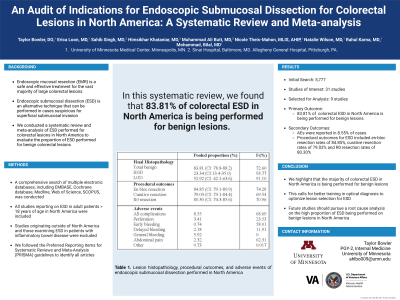
Introduction: Endoscopic mucosal resection (EMR) is a safe and effective treatment for the vast majority of large colorectal lesions. Endoscopic submucosal dissection (ESD) can be performed in cases suspicious for superficial submucosal invasion. This decision is often operator-dependent and based on optical diagnosis of polyp morphology and surface vascular and pit pattern. Here, we conduct a systematic review and meta-analysis of ESD performed for colorectal lesions in North America to evaluate the proportion of ESD performed for benign colorectal lesions.
Methods: A comprehensive literature search of multiple electronic databases was conducted from inception through May 2024 to identify all studies assessing ESD for colorectal lesions. Studies originating outside of North America and those examining ESD in patients with inflammatory bowel disease were excluded. The primary outcome was pooled proportion of ESD performed for benign colorectal lesions based on histopathology. Benign lesions were defined as lesions with low-grade and high-grade dysplasia. Secondary outcomes included procedure-related outcomes and adverse events (AEs) of ESD.
Results: Out of 5,777 citations, a total of 9 studies were included. Study population consisted of 1095 patients (mean age 64.3 years, 72.5% males). A total of 1095 colorectal lesions (mean size 41.97 mm) located in the rectum (n=583), right colon (n=340), and left colon (n=117) underwent ESD. Table 1 outlines the procedural related outcomes of ESD in North American studies. Pooled proportion of ESD for benign lesions was 83.81% (95% CI: 78.8-88.2; I2 72.60%). Pooled proportion of ESD for low-grade dysplasia was 52.92% (95% CI: 42.1-63.6; I2 91.10%), while pooled proportion for high-grade dysplasia was 23.34% (95% CI: 13.4-35.0; I2 93.77%). AEs were reported in 8.55% (95% CI: 5.5-12.1; I2 68.69%) of cases overall. The most commonly reported AEs included perforation, bleeding, and abdominal pain.
Discussion: In this meta-analysis, we demonstrate that the majority of colorectal ESD in North America is being performed for benign lesions. While ESD achieves high en-bloc and R0 resection rates, the risk of AEs is substantial. This calls for better training in optical diagnosis to optimize lesion selection for ESD, thereby minimizing the unnecessary risk associated with ESD for benign colorectal lesions. We recommend that future studies pursue a root cause analysis on the high proportions of ESD being performed on benign lesions in North America.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taylor Bowler, DO1, Erica Loon, DO2, Sahib Singh, MD3, Himsikhar Khataniar, MD4, Muhammad Ali Butt, MD4, Nicole Theis-Mahon, 2, Rahul Karna, MD2, Natalie Wilson, MD2, Mohammad Bilal, MD5. P1071 - An Audit of Indications for Endoscopic Submucosal Dissection for Colorectal Lesions in North America: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3Sinai Hospital, Baltimore, MD; 4Allegheny General Hospital, Pittsburgh, PA; 5University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Endoscopic mucosal resection (EMR) is a safe and effective treatment for the vast majority of large colorectal lesions. Endoscopic submucosal dissection (ESD) can be performed in cases suspicious for superficial submucosal invasion. This decision is often operator-dependent and based on optical diagnosis of polyp morphology and surface vascular and pit pattern. Here, we conduct a systematic review and meta-analysis of ESD performed for colorectal lesions in North America to evaluate the proportion of ESD performed for benign colorectal lesions.
Methods: A comprehensive literature search of multiple electronic databases was conducted from inception through May 2024 to identify all studies assessing ESD for colorectal lesions. Studies originating outside of North America and those examining ESD in patients with inflammatory bowel disease were excluded. The primary outcome was pooled proportion of ESD performed for benign colorectal lesions based on histopathology. Benign lesions were defined as lesions with low-grade and high-grade dysplasia. Secondary outcomes included procedure-related outcomes and adverse events (AEs) of ESD.
Results: Out of 5,777 citations, a total of 9 studies were included. Study population consisted of 1095 patients (mean age 64.3 years, 72.5% males). A total of 1095 colorectal lesions (mean size 41.97 mm) located in the rectum (n=583), right colon (n=340), and left colon (n=117) underwent ESD. Table 1 outlines the procedural related outcomes of ESD in North American studies. Pooled proportion of ESD for benign lesions was 83.81% (95% CI: 78.8-88.2; I2 72.60%). Pooled proportion of ESD for low-grade dysplasia was 52.92% (95% CI: 42.1-63.6; I2 91.10%), while pooled proportion for high-grade dysplasia was 23.34% (95% CI: 13.4-35.0; I2 93.77%). AEs were reported in 8.55% (95% CI: 5.5-12.1; I2 68.69%) of cases overall. The most commonly reported AEs included perforation, bleeding, and abdominal pain.
Discussion: In this meta-analysis, we demonstrate that the majority of colorectal ESD in North America is being performed for benign lesions. While ESD achieves high en-bloc and R0 resection rates, the risk of AEs is substantial. This calls for better training in optical diagnosis to optimize lesion selection for ESD, thereby minimizing the unnecessary risk associated with ESD for benign colorectal lesions. We recommend that future studies pursue a root cause analysis on the high proportions of ESD being performed on benign lesions in North America.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taylor Bowler indicated no relevant financial relationships.
Erica Loon indicated no relevant financial relationships.
Sahib Singh indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Muhammad Ali Butt indicated no relevant financial relationships.
Nicole Theis-Mahon indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant.
Taylor Bowler, DO1, Erica Loon, DO2, Sahib Singh, MD3, Himsikhar Khataniar, MD4, Muhammad Ali Butt, MD4, Nicole Theis-Mahon, 2, Rahul Karna, MD2, Natalie Wilson, MD2, Mohammad Bilal, MD5. P1071 - An Audit of Indications for Endoscopic Submucosal Dissection for Colorectal Lesions in North America: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
