Sunday Poster Session
Category: Interventional Endoscopy
P1072 - Predicting Factors of Higher Weight Loss After Endoscopic Transoral Outlet Reduction (TORe) in a Large Cohort of Bariatric Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RD
Ruvimbo Dzvurumi, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Elizza E. Villarruel, BS1, Fadi Dahoud, BS2, Ruvimbo Dzvurumi, BS2, Norman Spivak, BS2, Firas Bahdi, MD2, Maryam Farooq, BS2, Basak Kanlilar-Ruiz, NP2, Manar Alhanaee, MD2, Stephen Kim, MD2, Alireza Sedarat, MD2, Venkataraman R. Muthusamy, MD3, Adarsh Thaker, MD2, Danny Issa, MD2
1David Geffen School of Medicine at UCLA, La Puente, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Sherman Oaks, CA
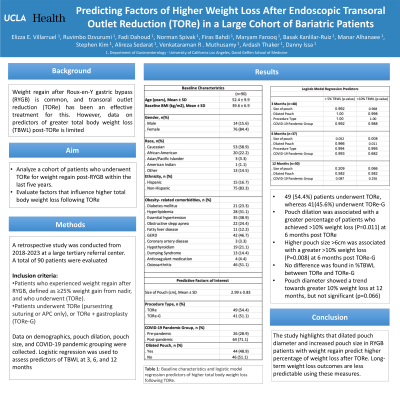
Introduction: Weight regain is a common complication following roux-en y gastric bypass (RYGB). While endoscopic transoral outlet reduction (TORe) is a safe and effective treatment for weight regain post RYGB, data on the factors predicting higher procedural efficacy is limited to a few centers and small studies. This study aimed to 1) analyze a cohort of patients who underwent TORe for weight regain within the last five years and 2) evaluate factors that influence higher total body weight loss (TBWL) following TORe.
Methods: A retrospective study was conducted using a prospectively maintained database of bariatric patients followed for five years (2018-2023) at a large tertiary-care referral center. Inclusion criteria were adult patients who experienced weight regain after RYGB, defined as ≥25% weight gain from nadir, and who underwent TORe. Patients underwent TORe (pursestring suturing or APC only), or TORe + gastroplasty (TORe-G). Demographic and procedural variables were collected. Primary outcomes were factors that predicted >5% and >10% TBWL after TORe. Secondary outcomes included %TBWL at 3, 6, and 12 months after TORe.
Results: A total of 90 RYGB patients who underwent TORe (mean age 52.4 ± 9.9, baseline BMI: 39.6 ± 6.9) were evaluated. 49(54.4%) patients underwent TORe, whereas 41 (45.6%) underwent TORe-G. Logistic regression analysis showed two primary predictors of higher weight loss. Pouch dilation was associated with a greater percentage of patients who achieved >10% weight loss (P=0.011) at 6 months post TORe. Similarly, higher pouch size >6cm was associated with a greater >10% weight loss (P=0.008) at 6 months post TORe-G. After adjusting for size/pouch diameters, no difference was found in %TBWL between the TORe and TORe-G. Pouch diameter showed a trend towards greater 10% weight loss at 12 months, but no significance (p=0.066). A trend was observed towards >5% weight loss at 12 months in patients treated post-COVID-19 pandemic compared to pre-pandemic (p = 0.087).
Discussion: The study highlights that dilated pouch diameter and increased pouch size in RYGB patients with weight regain predict higher percentage of weight loss after TORe. Long-term weight loss outcomes are less predictable using these measures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elizza E. Villarruel, BS1, Fadi Dahoud, BS2, Ruvimbo Dzvurumi, BS2, Norman Spivak, BS2, Firas Bahdi, MD2, Maryam Farooq, BS2, Basak Kanlilar-Ruiz, NP2, Manar Alhanaee, MD2, Stephen Kim, MD2, Alireza Sedarat, MD2, Venkataraman R. Muthusamy, MD3, Adarsh Thaker, MD2, Danny Issa, MD2. P1072 - Predicting Factors of Higher Weight Loss After Endoscopic Transoral Outlet Reduction (TORe) in a Large Cohort of Bariatric Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, La Puente, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Sherman Oaks, CA
Introduction: Weight regain is a common complication following roux-en y gastric bypass (RYGB). While endoscopic transoral outlet reduction (TORe) is a safe and effective treatment for weight regain post RYGB, data on the factors predicting higher procedural efficacy is limited to a few centers and small studies. This study aimed to 1) analyze a cohort of patients who underwent TORe for weight regain within the last five years and 2) evaluate factors that influence higher total body weight loss (TBWL) following TORe.
Methods: A retrospective study was conducted using a prospectively maintained database of bariatric patients followed for five years (2018-2023) at a large tertiary-care referral center. Inclusion criteria were adult patients who experienced weight regain after RYGB, defined as ≥25% weight gain from nadir, and who underwent TORe. Patients underwent TORe (pursestring suturing or APC only), or TORe + gastroplasty (TORe-G). Demographic and procedural variables were collected. Primary outcomes were factors that predicted >5% and >10% TBWL after TORe. Secondary outcomes included %TBWL at 3, 6, and 12 months after TORe.
Results: A total of 90 RYGB patients who underwent TORe (mean age 52.4 ± 9.9, baseline BMI: 39.6 ± 6.9) were evaluated. 49(54.4%) patients underwent TORe, whereas 41 (45.6%) underwent TORe-G. Logistic regression analysis showed two primary predictors of higher weight loss. Pouch dilation was associated with a greater percentage of patients who achieved >10% weight loss (P=0.011) at 6 months post TORe. Similarly, higher pouch size >6cm was associated with a greater >10% weight loss (P=0.008) at 6 months post TORe-G. After adjusting for size/pouch diameters, no difference was found in %TBWL between the TORe and TORe-G. Pouch diameter showed a trend towards greater 10% weight loss at 12 months, but no significance (p=0.066). A trend was observed towards >5% weight loss at 12 months in patients treated post-COVID-19 pandemic compared to pre-pandemic (p = 0.087).
Discussion: The study highlights that dilated pouch diameter and increased pouch size in RYGB patients with weight regain predict higher percentage of weight loss after TORe. Long-term weight loss outcomes are less predictable using these measures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elizza Villarruel indicated no relevant financial relationships.
Fadi Dahoud indicated no relevant financial relationships.
Ruvimbo Dzvurumi indicated no relevant financial relationships.
Norman Spivak: BrainSonix Corp – Consultant.
Firas Bahdi indicated no relevant financial relationships.
Maryam Farooq indicated no relevant financial relationships.
Basak Kanlilar-Ruiz indicated no relevant financial relationships.
Manar Alhanaee indicated no relevant financial relationships.
Stephen Kim: Boston Scientific – Consultant.
Alireza Sedarat indicated no relevant financial relationships.
Venkataraman Muthusamy: Boston Scientific – Consultant, Grant/Research Support. Capsovision – Stock Options, Stock-privately held company. Castle Biosciences – Consultant, Speakers Bureau. Endogastric Solutions – Advisory Committee/Board Member, Consultant, Speakers Bureau. Medtronic – Consultant. Pentax Medical – Consultant.
Adarsh Thaker: Boston Scientific Corporation – Consultant, Speakers Bureau. Cook – Speakers Bureau. Fractyl Health – Grant/Research Support. Neptune Medical – Consultant. Steris – Consultant.
Danny Issa: Boston Scientific – Consultant, Speakers Bureau. Eli Lilly – Speakers Bureau.
Elizza E. Villarruel, BS1, Fadi Dahoud, BS2, Ruvimbo Dzvurumi, BS2, Norman Spivak, BS2, Firas Bahdi, MD2, Maryam Farooq, BS2, Basak Kanlilar-Ruiz, NP2, Manar Alhanaee, MD2, Stephen Kim, MD2, Alireza Sedarat, MD2, Venkataraman R. Muthusamy, MD3, Adarsh Thaker, MD2, Danny Issa, MD2. P1072 - Predicting Factors of Higher Weight Loss After Endoscopic Transoral Outlet Reduction (TORe) in a Large Cohort of Bariatric Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
